Is Long-term Beta-blocker Therapy Needed after a Heart Attack?

For patients with a history of myocardial infarction (MI), cardiovascular safety of interrupting beta-blocker could not be shown in comparison to continuation and there was no benefit to the patients’ quality of life, according to late-breaking research presented in a Hot Line session today at ESC Congress 2024.1
“Improvements in MI management and data from observational studies have led physicians to question whether continuing beta-blockers after one year post-MI is needed since unnecessary treatment may result in side effects.2-5 We conducted the ABYSS trial to provide conclusive randomised data on the effects of beta-blocker interruption vs. continuation on cardiovascular events and quality of life, but we were unable to show safety preservation in terms of clinical events nor any benefit on quality of life with beta-blocker interruption,” said Principal Investigator, Professor Johanne Silvain of the Sorbonne University, Paris, France.
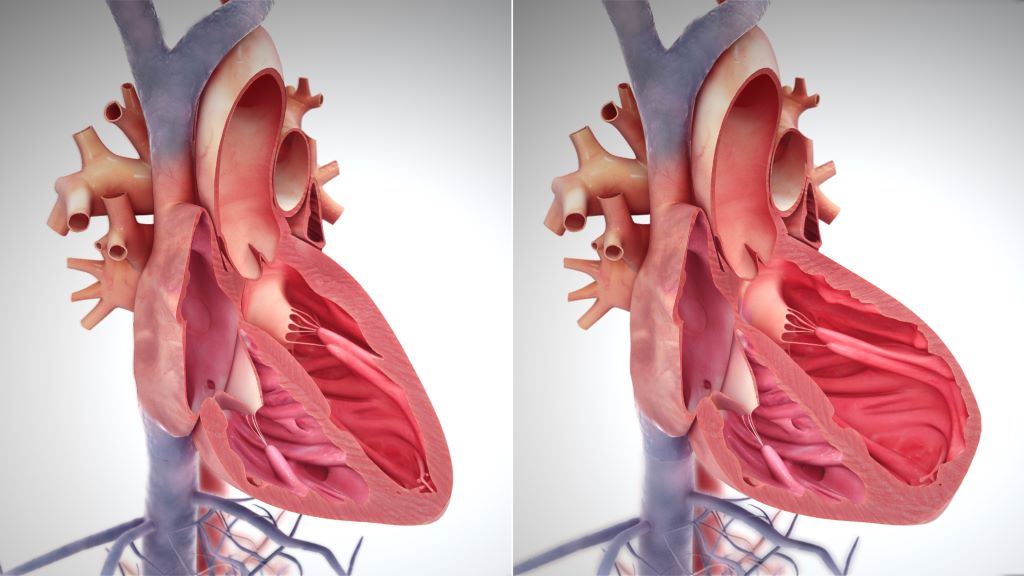
The open-label, non-inferiority, randomised ABYSS trial, conducted by the ACTION Group, included patients with a prior MI taking long-term beta-blockers, with a left ventricular ejection fraction of at least 40% and no cardiovascular events in the previous six months. Participants were randomised (1:1) to interrupting or continuing their β-blocker medication.
The primary endpoint was a composite of death, non-fatal MI, non-fatal stroke or hospitalisation for cardiovascular reasons at the longest follow-up (minimum, one year), according to an analysis of non-inferiority (defined as a between-group absolute difference of < 3 percentage points for the upper boundary of the two-sided 95% confidence interval [CI]). The main secondary endpoint was the change in quality of life as measured by the European Quality of Life–5 Dimensions questionnaire.
In total 3698 patients were randomised from 49 sites in France. The mean age was 64 years and 17% were female. The median time between last MI and randomisation was 2.9 years (interquartile range 1.2–6.4 years).
Over median follow-up of 3 years, interruption of long-term beta-blocker treatment was not shown to be non-inferior to beta-blocker continuation. A primary-outcome event occurred in 23.8% of patients in the interruption group and in 21.1% in the continuation group (risk difference 2.8 percentage points; 95% CI <0.1–5.5), with a hazard ratio of 1.16 (95% CI 1.01–1.33; p = 0.44 for non-inferiority).
Death occurred in 4.1% in the interruption group and 4.0% in the continuation group, while MI occurred in 2.5% and 2.4%, respectively. Of note, hospitalisation for cardiovascular causes occurred in 18.9% in the interruption group and 16.6% in the continuation group. Beta-blocker interruption was also associated with increases in systolic and diastolic blood pressure and heart rate at 6 months (all p<0.001 vs. beta-blocker continuation) and during the study follow up. Beta-blocker interruption did not improve the patients’ quality of life.
Summing up the evidence from the ABYSS trial, Professor Silvain concluded: “Differences between the groups with respect to hospitalisation for cardiovascular reasons and the negative effect on blood pressure levels, together with the absence of quality-of-life improvement do not support interruption of a chronic beta-blocker treatment in post-MI patients. These results must be put into context with recent findings from the open-label REDUCE-MI6 trial and ongoing trials to provide additional evidence on the optimal use of beta-blockers after MI.”
References
- ‘Beta blocker interruption in patients with prior myocardial infarction: results of the ABYSS trial and effect on blood pressure and heart rate control’ will be discussed during Hot Line 1 on Friday 30 August in room London.
- Holt A, Blanche P, Zareini B, et al. Effect of long-term beta-blocker treatment following myocardial infarction among stable, optimally treated patients without heart failure in the reperfusion era: a Danish, nationwide cohort study. Eur Heart J. 2021;42:907–914.
- Park CS, Yang H-M, Ki Y-J, et al. Left ventricular ejection fraction 1 year after acute myocardial infarction identifies the benefits of the long-term use of beta-blockers: analysis of data from the KAMIR-NIH Registry. Circ Cardiovasc Interv. 2021;14:e010159.
- Puymirat E, Riant E, Aissaoui N, et al. β Blockers and mortality after myocardial infarction in patients without heart failure: multicentre prospective cohort study. BMJ. 2016;354:i4801.
- Kim J, Kang D, Park H, et al. Long-term β-blocker therapy and clinical outcomes after acute myocardial infarction in patients without heart failure: nationwide cohort study. Eur Heart J. 2020;41:3521–3529.
- Yndigegn T, Lindahl B, Mars K, et al. Beta-blockers after myocardial infarction and preserved ejection fraction. N Engl J Med. 2024;390:1372–1381.
Source: European Society of Cardiology