Diabetes Can Drive the Evolution of Antibiotic Resistance

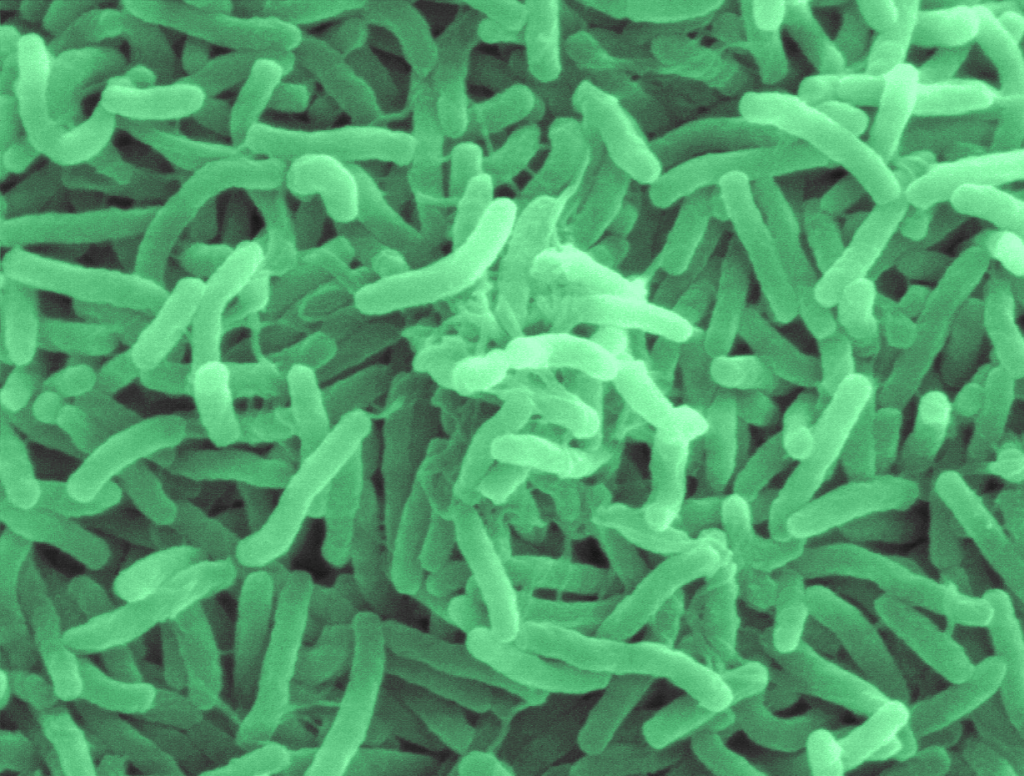
Staphylococcus aureus is a leading cause of antibiotic resistance associated infections and deaths. It is also the most prevalent bacterial infection among those with diabetes mellitus, a chronic condition that affects blood sugar control and reduces the body’s ability to fight infections.
Microbiologists at the UNC School of Medicine have just shown that people with diabetes are more likely to develop antibiotic-resistant strains of Staph, too. Their results, which were published in Science Advances, show how the diabetic microbial environment produces resistant mutations, while hinting at ways antibiotic resistance can be combatted in this patient population.
“We found that antibiotic resistance emerges much more rapidly in diabetic models than in non-diabetic models of disease,” said Brian Conlon, PhD, associate professor of immunology. “This interplay between bacteria and diabetes could be a major driver of the rapid evolution and spread of antibiotic resistance that we are seeing.”
Staph feeds off the high levels of blood glucose in diabetes, allowing it to reproduce more rapidly. The bacterium can also grow without consequence, as diabetes also impairs the immune system’s ability to destroy cells and control infection.
As the numbers of bacteria increase in a diabetic infection, so does the likelihood of resistance. Random mutations appear and some build up resistance to external stressors, like antibiotics. Once a resistant mutant is present in a diabetic infection, it rapidly takes over the population, using the excess glucose to drive its rapid growth.
“Staphylococcus aureus is uniquely suited to take advantage of this diabetic environment,” said Lance Thurlow, PhD, assistant professor of microbiology and immunology. “Once that resistant mutation happens, you have excess glucose and you don’t have the immune system to clear the mutant and it takes over the entire bacterial population in a matter of days.”
Conlon, an expert on antibiotic treatment failure, and Thurlow, an expert on Staph pathogenesis in diabetes, have long been interested in comparing the effectiveness of antibiotics in a model with and without diabetes. Using their connections within the Department of Microbiology and Immunology, the researchers brought their labs together to perform a study with antibiotics in a diabetic mouse model of S. aureus infection.
First, the team prepared a mouse model with bacterial infection in the skin and soft tissue. The mouse models were divided into two groups: one half was given a compound that selectively kills cells in the pancreas, rendering them diabetic, and the other half was not given the compound. Researchers then infected both diabetic and non-diabetic models with S. aureus and treated them with rifampicin, an antibiotic where resistance evolves at a high rate.
After five days of infection, it was time to observe the results.
Conlon and Thurlow were quick to notice that the rifampicin had practically no effect in diabetic models. So, they took some samples to investigate. Researchers were shocked to find that the bacteria had evolved to become resistant to rifampicin, with the infection harboring over a hundred million rifampicin resistant bacteria. There were no rifampicin resistant bacteria in the non-diabetic models.
Their new findings have left Conlon and Thurlow with many questions; however, they are certain that the evolution of antibiotic resistance in people with diabetes could spell trouble for the population at large.
And, even more surprisingly, the mutation had taken over the entire infection in just four days. They next inoculated diabetic and non-diabetic models with Staphylococcus aureus as before, but this time supplemented with a known number of rifampicin resistant bacteria. Again, these bacteria rapidly took over the diabetic infection, but remained as only a sub-population in non-diabetic models after 4 days rifampicin treatment.
Their new findings have left Conlon and Thurlow with many questions; however, they are certain that the evolution of antibiotic resistance in people with diabetes could spell trouble for the population at large. Antibiotic-resistant strains of bacteria spread from person to person in the same ways as other bacteria and viruses do – in the air, on doorknobs, and the food that we eat – which makes preventing these types of infections a major priority.
So, what can be done to prevent it? Well, the Conlon and Thurlow labs showed that reducing blood sugar levels in diabetic models (through administration of insulin) deprived bacteria of their fuel, keeping their numbers at bay, and reducing the chances of antibiotic-resistant mutations from occurring. Their findings suggest that controlling blood sugar through insulin use could be key in preventing antibiotic resistance.
“Resistance and its spread are not only associated with the prescription of drugs, but also the health status of those that are taking antibiotics,” said Conlon. “Controlling blood glucose then becomes really important. When we gave our mice insulin, we were able to bring their blood sugar back to normal and we didn’t get this rapid proliferation of resistant bacteria.”
Now, Conlon and Thurlow are expanding their efforts to study the evolution of resistance in humans (with and without diabetes) and other antibiotic-resistant bacteria of interest, including Enterococcus faecalis, Pseudomonas aeruginosa, and Streptococcus pyogenes. Recognizing how large a role the host plays a role in the evolution of antibiotic resistance, the researchers plan to perform similar studies in patients undergoing chemotherapy and recent transplant recipients to see if those populations are also prone to antibiotic resistant infections.