It is a Time for Solutions, Says Prof Tulio de Oliveira in Face of US Funding Cuts

Cuts to United States spending on aid and medical research have caused widespread havoc and anxiety in the last month. Professor Tulio de Oliveira sat down with Spotlight’s Biénne Huisman to talk through what it might mean for health research in South Africa.
As the Trump administration moves to freeze foreign aid, halting vital humanitarian health programmes and medical research trials worldwide – leaving patients cut off from lifesaving medicines and scientists in a bind – Professor Tulio de Oliveira argues that the United States stand to lose far more from this move than its 1% government investment in foreign aid.
The non-partisan Pew Research Center recently released figures showing that of the American government’s total 2023 budget, 1.2% or about $71.9 billion was spent on foreign aid. Of this foreign aid budget, 14.7% or about $10.6 billion was earmarked for the “ongoing battle against HIV/AIDS” and 2% or about $1.5 billion for “combatting pandemic influenza and other emerging public health threats”.
Speaking to Spotlight in a boardroom at the Centre for Epidemic Response and Innovation (CERI) at Stellenbosch University, De Oliveira says: “Spending on biosecurity is an investment in the future – I think the United States benefits much more from our research and our work than what we cost them.” Biosecurity refers to measures designed to protect populations against harmful biological or biochemical substances.
During the height of the COVID-19 pandemic, De Oliveira, a professor in bioinformatics, shot to global attention for leading the South African team credited with discovering the Beta and Omicron variants of SARS-CoV-2. Now, in the face of a new global health upheaval, he insists that cross-border scientific collaboration is critical for combating the global spread of disease.
“Pathogens don’t need passports, they don’t care about nationality,” he says, referencing former World Health Organisation Director-General, Dr Margaret Chan, who first used the phrase at the 2007 World Health Assembly.

De Oliveira is a native Brazilian who speaks accented English. During his interview with Spotlight, his demeanour is calm and his speech unrushed as he expands: “It’s of great interest to America to keep investing – not as a kind of donation, or because we’re entitled to it – but because of how it helps them. We just came out of a pandemic and America actually had much bigger waves of infection than many of the poor countries.”
He lists recent global population health threats: “Like with Covid, now we have influenza; and the virus is mutating, transmitting through multiple animals. We just had an outbreak of Marburg in Rwanda and another one in Kenya. We had an emergence of mpox in central Africa. We had an emergence in Sudan of a strain of Ebola. In Uganda, a growing rate of malaria drug resistance.
“And in the last year, the US saw the biggest number of TB cases ever. So it’s of critical interest that these pathogens get quickly identified, are quickly controlled, that you treat people so that it doesn’t spread to other countries. In the end, it’s the health of the global population, it doesn’t matter which country we live in or how wealthy people are.”
Major funding cuts
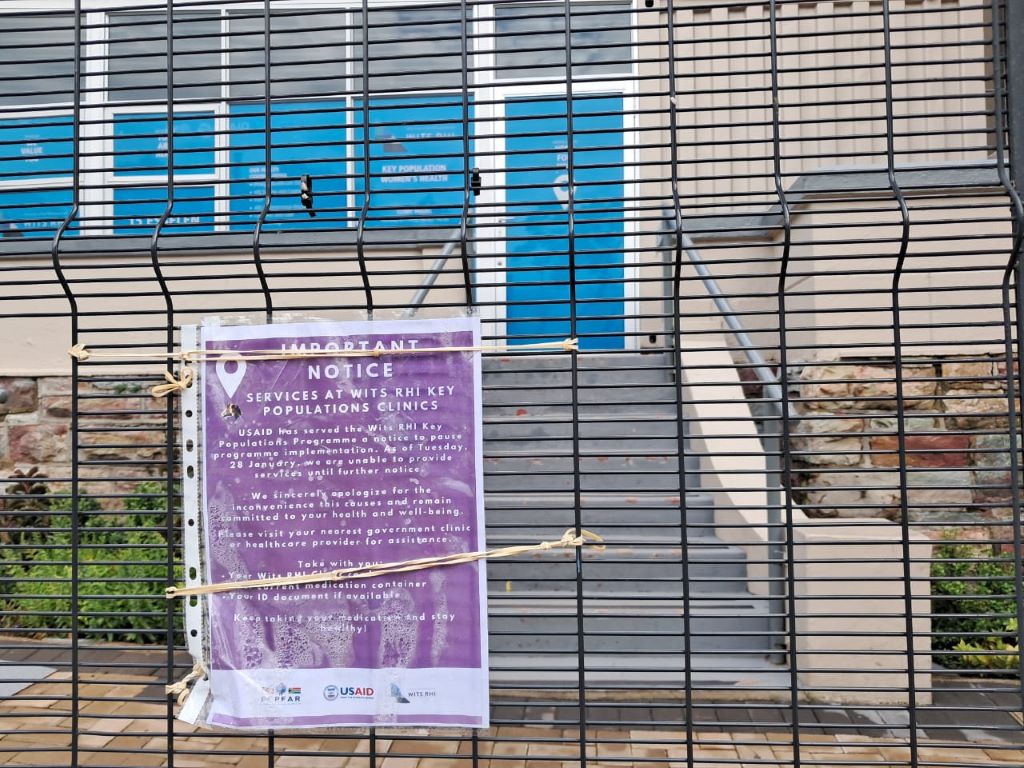
Scores of South African research groups (many who provide affiliated public healthcare services) have in the past received funding from United States government entities – including the National Institutes of Health (NIH), the Centers for Disease Control and Prevention (CDC), USAID, and the President’s Emergency Plan for Aids Relief (PEPFAR).
Many of these funding flows have been paused in recent weeks by the Trump administration. As a result, several important clinical trials have been stopped. The impacts are far-reaching – around 28% of the South African Medical Research Council’s (SAMRC) 2025/2026 budget was set to be funded by US government entities. Professor Ntobeko Ntusi, President of the SAMRC, told Spotlight that it would be catastrophic if the funding is cut.
Adding further uncertainty, prominent vaccine sceptic Robert F. Kennedy has been confirmed as the US’s health secretary under the Trump administration. Kennedy has argued that the NIH should reduce its focus on infectious diseases and dedicate more resources to non-communicable diseases like diabetes. The US government has until now been by far the biggest funder of both HIV and TB research.
De Oliveira appears unflustered. At CERI, of which he is the founding director, he says only 7% of funding is from the NIH – “and we have reason to believe that the current NIH grants that we have will not be discontinued”. One such grant was for R40 million over five years awarded in 2023 to CERI’s Professor Frank Tanser for designing HIV prevention strategies.
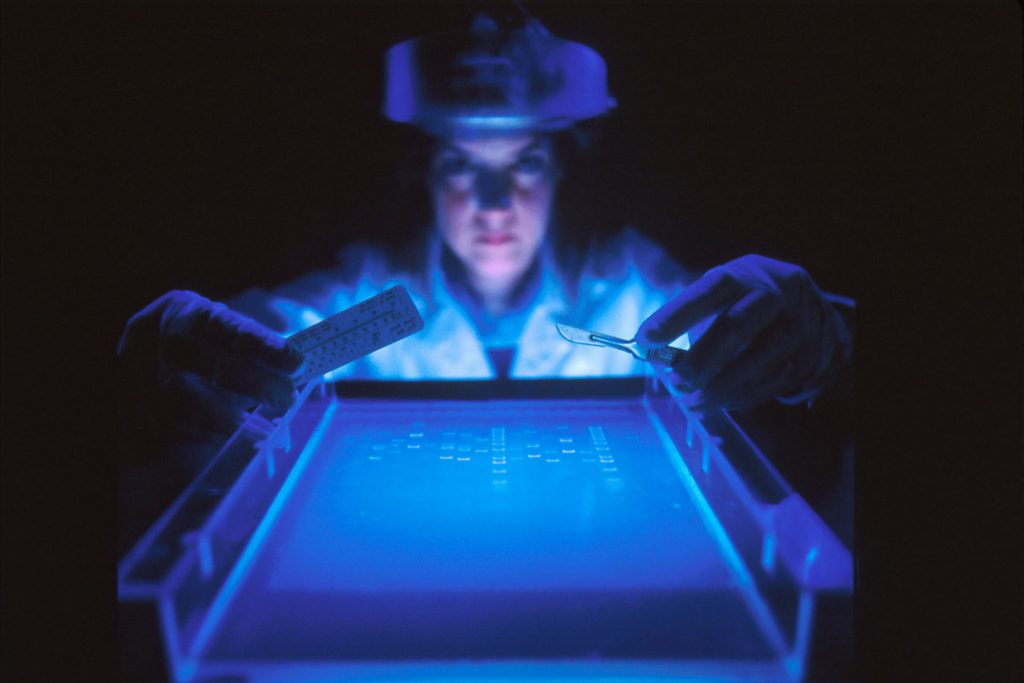
In fact, De Oliveira says CERI and the KwaZulu-Natal Research Innovation and Sequencing Platform (KRISP) which he also heads, are expanding. Both centres use state-of-the-art genomics – the study of the DNA of organisms – to identify new variants of pathogens and to prevent disease.
“Yes, the opposite, we’re in an expansion phase,” says De Oliveira.
“Just last week, we advertised five post-doctoral fellowship positions. We hope that we can even absorb some of the great talent that may be lost from groups that were unfortunately more reliant on American funding.”
He stresses the importance of having a diversified funding portfolio, saying the work of CERI and KRISP is funded through 46 active grants with another 9 in the offing. “We have multiple grants from multiple funders from multiple countries. So again, I know it’s easily said, but I think it’s something that we should learn going forward, not to grow too reliant on one funder.”
Filling the gap
If the United States pulls back permanently from its leadership role in providing global aid – and medical research funding in particular – who might fill the gap?
The New Yorker quotes Clemence Landers, vice-president of the think tank Centre for Global Development, suggesting that China might come forward.
In response, De Oliveira says: “China could fill the gap. But people don’t realise the biggest foundation in the world at the moment is called the Novo Nordisk Foundation in Denmark which is linked to the company that had the massive breakthrough with Ozempic. They could easily fill the gap if they wanted. There are others as well. I would not be surprised if a completely unexpected foundation came forward to fill the gap.”
Reflecting further, he expresses hope that “people with noble causes step up”.
In 2022, TIME Magazine named De Oliveira one of the world’s 100 most influential people, and in 2024 he cracked the magazine’s top 100 health list. Has this public recognition made it easier for him to attract funding? He shrugs this off.
“We’re really committed to having a global impact that saves lives. And that commitment is not centralised in the director, but in our vision shared across principal investigators. And this is really important for the sustainability of organisations. I get offered good jobs every couple of weeks, and I mean even though I don’t intend on going anywhere, anything could happen. For example, two weeks ago I was skateboarding and cracked my ribs.”
In a moment of levity, he elaborates: “And this is the fifth time I cracked my ribs. Once was while skateboarding, another while snowboarding, surfing, once while mountain biking and another time falling from a children’s tractor.”
De Oliveira moved to South Africa in 1997, as the AIDS crisis was heading toward its peak. He says he feels “eternally grateful” for the boost PEPFAR brought to South Africa’s HIV-programme, adding that today the country might be in a “better position to absorb the loss of the funding than say five, ten years ago”.
He notes that 17% of South Africa’s HIV/AIDS spending was from PEPFAR, but that this does not include the procurement of antiretrovirals. “So yes, I think as South Africans we might be in a position to come up with solutions, as the programme is very well run.”
De Oliveira’s concern is for more vulnerable African countries – he singles out Mozambique – which are reliant on foreign aid for the procurement of medicines like antiretrovirals.
Needless to say, these recent events are a setback in the quest to develop an HIV vaccine. “When you decrease investment in research and science, you keep further away from developing the solutions,” he says. “But in terms of HIV/AIDS, luckily there are antiretroviral therapies that are very efficient.”
As we wrap up the interview, De Oliveira zooms out to the bigger picture: “Unfortunately, we are destroying the environment, there’s increased globalisation and crazy urbanisation, and this is making it easier for infectious diseases to spread.
“This is a challenging time for scientific and medical research. A time to develop solutions.”
Republished from Spotlight under a Creative Commons licence.
Read the original article.