Research reports for the first time a pathway that begins in the gut and ends with a potent pro-inflammatory toxin in brain cells contributing to the development of Alzheimer’s disease (AD). Results are published in Frontiers in Neurology, where the researchers also report a simple way to counter the process.
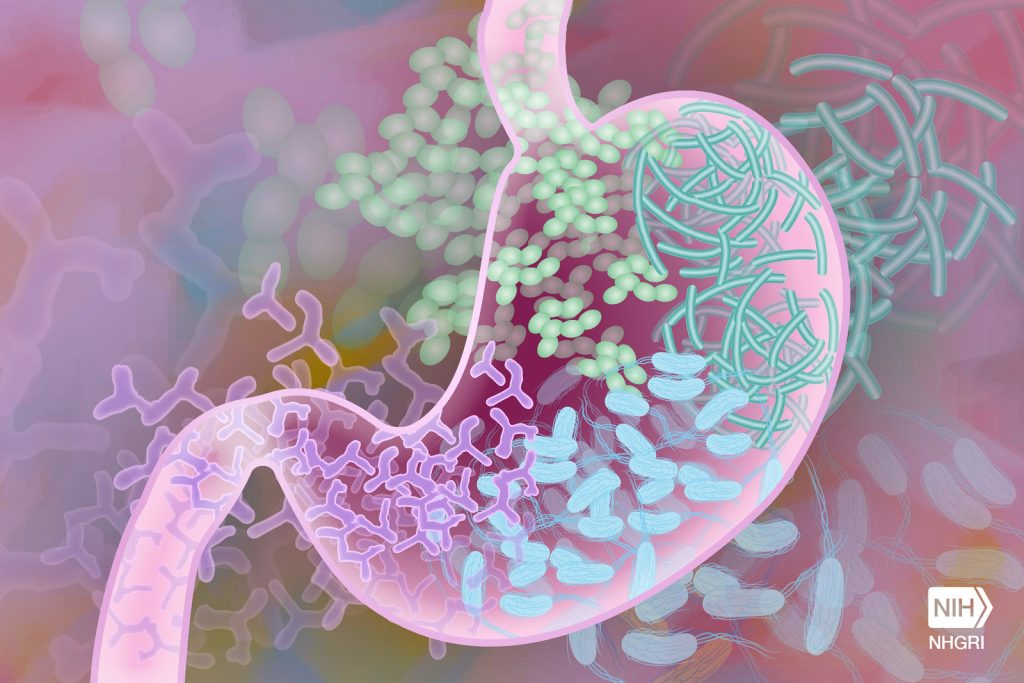
The researchers, led by Drs Yuhai Zhao and Walter J Lukiw, found evidence that a molecule containing a very potent microbial-generated neurotoxin (lipopolysaccharide or LPS) derived from the Gram-negative bacteria Bacteroides fragilis in the human gastrointestinal (GI) tract generates a neurotoxin known as BF-LPS.
“LPSs in general are probably the most potent microbial-derived pro-inflammatory neurotoxic glycolipids known,” explained Dr Lukiw. “Many laboratories, including our own, have detected different forms of LPS within neurons of the Alzheimer’s disease-affected human brain.”
The researchers detailed the pathway of BF-LPS from the gut to the brain and its mechanisms of action once there. BF-LPS leaks out of the GI tract, crosses the blood brain barrier via the circulatory system, and accesses brain compartments. Then it increases inflammation in brain cells and inhibits neuron-specific neurofilament light (NF-L,) a protein that supports cell integrity. A deficit of this protein leads to progressive neuronal cell atrophy, and ultimately cell death, as is observed in AD-affected neurons. They also report that adequate intake of dietary fibber can head off the process.
The novel features of this newly described pathological pathway are threefold. The AD-stimulating pathway begins in the gut microbiome and therefore is very “locally sourced” and active throughout our lives. The highly potent neurotoxin BF-LPS is a natural by-product of gut-based microbial metabolism. Bacteroides fragilis abundance in the microbiome, which is the source of the neurotoxin BF-LPS, can be regulated by dietary fiber intake.
“Put another way, dietary-based approaches to balance the microorganisms in the microbiome may be an attractive means to modify the abundance, speciation, and complexity of enterotoxigenic forms of AD-relevant microbes and their potential for the pathological discharge of highly neurotoxic microbial-derived secretions that include BF-LPS and other forms of LPS,” Dr Lukiw explained.
The researchers conclude that an improved understanding of the interaction between the Gut–Brain axis and the gut microbiome and Alzheimer’s disease has considerable potential to lead to new diagnostic and therapeutic strategies in the clinical management of Alzheimer’s disease and other lethal, progressive, and age-related neurodegenerative disorders.

