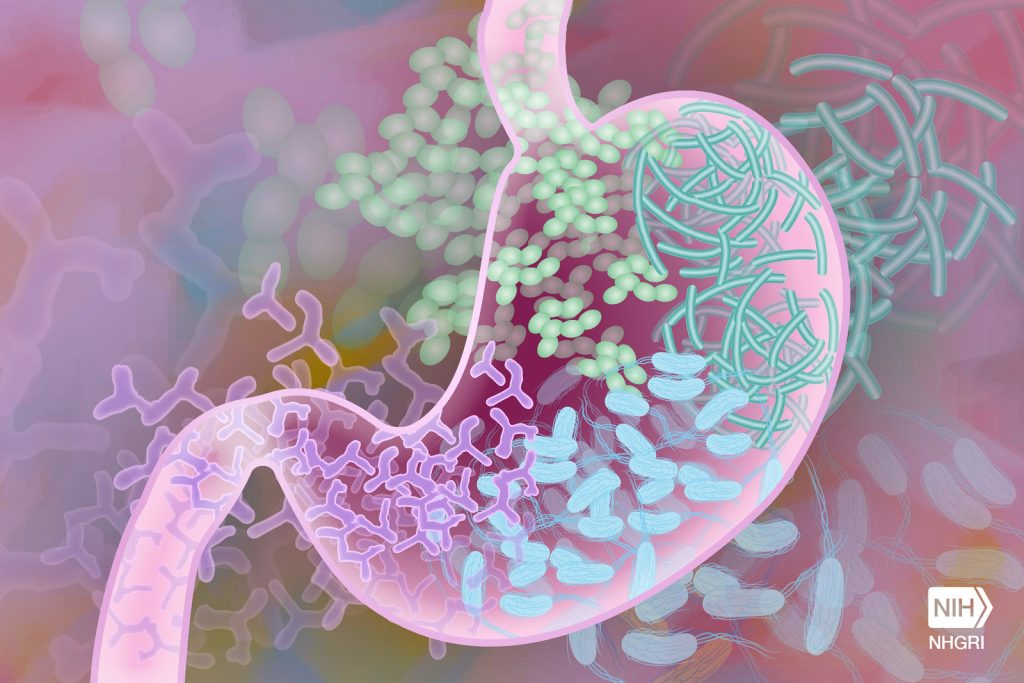
The gut microbiome has been linked to aspects ranging from the immune system to mental health. However, pinpointing how and which bacteria specifically affect which biological process has eluded researchers, until now – a new study figured it out the link between immunity and a major gut bacterium.
Such knowledge is essential for learning how to manipulate gut bacteria to treat or prevent illness.
“Microbiome studies need to move from making associations to determining function and causation,” said Professor Ramnik Xavier, co-author of the study which appears in Nature.
“The real significance of this work was connecting a bacterium, the molecule it makes, the pathway it operates through, and the biological outcome,” said Professor at HMS and co-senior author of the study with Prof Xavier. “That’s very rare.”
Profs Clardy and Xavier and colleagues focused on Akkermansia muciniphila, a species that makes up 3% of the gut microbiome. It gets its name from the intestinal mucus it breaks down.
Studies had suggested that A. muciniphila has a key role in maintaining healthy immune processes, seeming to protect against diseases such as type 2 diabetes and inflammatory bowel disease and make cancer cells more responsive to immune checkpoint therapies. Until now, no research could confirm how that connection worked.
Start to finish
The researchers show that the links begin with a lipid in A. muciniphila‘s cell membrane.
“That discovery was quite surprising. The usual suspects for triggering an immune response would be a protein or a sugar,” said Prof Clardy.
After discovering the molecular structure of the lipid, the team found that it communicates toll-like receptors (TLR) 2 and TLR 1. Found on many immune cells, they detect bacteria and identify hostile ones for the immune system. In this case, versions of TLR2 and TLR1 bound together in a way scientists hadn’t seen before.
The researchers showed in cell cultures that the fat’s activation of TLR2-TLR1 can trigger the release of certain cytokines — immune proteins involved in inflammation — while leaving other cytokines alone.
They also confirmed that the lipid helps maintain immune homeostasis. They found that low doses of the lipid act like a leash, preventing the immune system from reacting to a potentially harmful molecule until that molecule reaches significant levels. On the other end, they saw that high doses of the lipid don’t stimulate an immune response much more than low or medium doses, keeping a healthy ceiling on inflammation.
New doors open
The work introduces new possibilities for developing drugs that piggyback on A. muciniphila‘s ability to manipulate the immune system and fight disease. Members of Prof Clardy’s lab have made that job easier by revealing the molecular structure of the lipid and figuring out how scientists can make it and similar ones easily in the lab.
The study also serves as a model for pinpointing how other members of the gut microbiome act on the body.
“You can change the bacterium and apply the same set of tests,” said Prof Clardy.
Also, contrary to the expectations of many people in the field, such work doesn’t require fancy techniques. The researchers used traditional methods, spectroscopic analysis and chemical synthesis, to find and understand the lipid molecule.
In fact, despite its “remarkable activity,” the lipid has a “generic structure” that would have flown under the radar of more advanced genomic or metabolomic analyses, Prof Clardy said.
“The gut microbiome and the immune system are very complicated, which makes you expect that answers will be complicated too,” he said. “But sometimes complicated things are just lots of simple things.”
Source: Harvard Medical School

