Researchers at Massachusetts General Hospital (MGH) have discovered a network of brain regions activated by the placebo effect overlaps with several regions targeted by brain-stimulation therapy for depression.
The findings of this study, published in Molecular Psychiatry, will help in understanding the neurobiology of placebo effects and could inform how brain stimulation trial results are interpreted. In addition, this could provide insights on how to harness placebo effects for the treatment of a variety of conditions.
The placebo effect occurs when a patient’s symptoms improve because they expect a therapy to help (due to a variety of factors), but not from the specific effects of the treatment itself. Recent research indicates that there is a neurological basis for the placebo effect, with imaging studies identifying a pattern of changes that happen in certain brain regions when a person experiences this phenomenon.
The use of brain-stimulation techniques for patients with depression that doesn’t respond adequately to medication or psychotherapy has gained wider use in recent years. Transcranial magnetic stimulation (TMS) delivers electromagnetic pulses to the brain, and its effect on brain activity has been established over the last three decades in animal and human research studies, with several TMS devices approved by the Food and Drug Administration for treating depression. In addition, for treatment depression, deep brain stimulation (DBS, which requires an implanted device) has shown some promise.
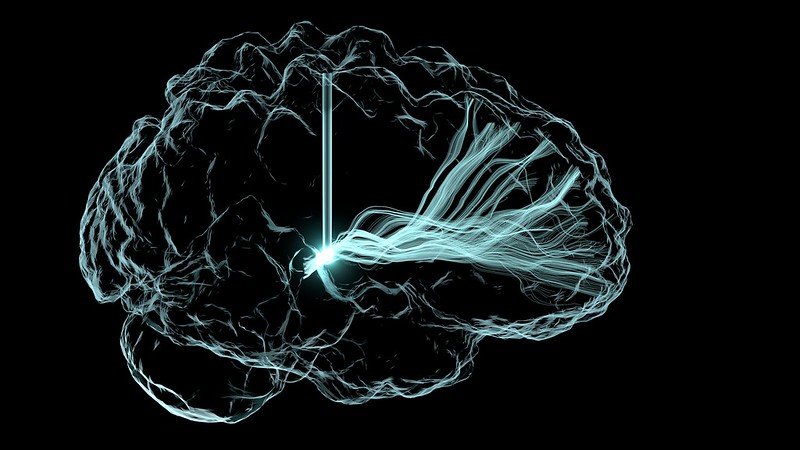
Senior author Emiliano Santarnecchi, PhD, saw studies of brain stimulation as a unique opportunity to learn more about the neurobiology of the placebo effect. Santarnecchi and his co-investigators conducted a meta-analysis and review of neuroimaging studies involving healthy subjects and patients to create a “map” of brain regions activated by the placebo effect. They also analysed studies of people treated with TMS and DBS for depression to identify brain regions targeted by the therapies. The team found that several sites in the brain that are activated by the placebo effect overlap with brain regions targeted by TMS and DBS.
Dr Santarnecchi and his colleagues believe that this overlap has critical importance in interpreting the results of research on brain stimulation for conditions such as depression. In clinical trials, a significant portion of depression patients receiving brain stimulation improve — but so do many patients receiving placebo (sham) treatment, in which no stimulation is administered, which has led to confusion over the therapy’s benefits.
A possible explanation is “that there is a significant placebo effect when you do any form of brain stimulation intervention,” said Dr Santarnecchi. TMS involves a clinical setting, with loud clicks as the pulse is delivered. “So the patient thinks, ‘Wow, they are really activating my brain’, so you get a lot of expectation,” said Dr Santarnecchi.
Elevated placebo effects associated with brain stimulation may create problems when studying the intervention, said first author Matthew Burke, MD, a cognitive neurologist. If brain stimulation and the placebo effect overlap in activating the same brain regions, then those circuits could be maximally activated by placebo effects, which could make it difficult to show any additional benefit from TMS or DBS, said Dr Burke. If so, this could explain the disparity of results in neurostimulation treatment of depression. Screening out placebo from brain stimulation’s direct impact on brain activity will help in designing studies where the real potential of techniques such as TMS will be more easily quantified, thus improving the effect of treatment protocols.
The findings from this study also suggest broad applications for the placebo effect, said Dr Santarnecchi. “We think this is an important starting point for understanding the placebo effect in general, and learning how to modulate and harness it, including using it as a potential therapeutic tool by intentionally activating brain regions of the placebo network to elicit positive effects on symptoms,” he said.
Dr Santarnecchi and his colleagues are currently designing trials that they hope will “disentangle” the effects of brain stimulation from placebo effects and offer insights about how they can be leveraged in clinical settings.
Source: Massachusetts General Hospital

