The Hammanskraal cholera outbreak continues with 17 deaths from the disease reported so far. Poverty is exacerbating the situation, with residents being advised to drink bottled water – but unable to afford it. According to GroundUp, the microbiological compliance (a measure of faecal bacteria) at sewage treatment plants was as low as 2% and 0%, where below 50% is considered ‘bad’.
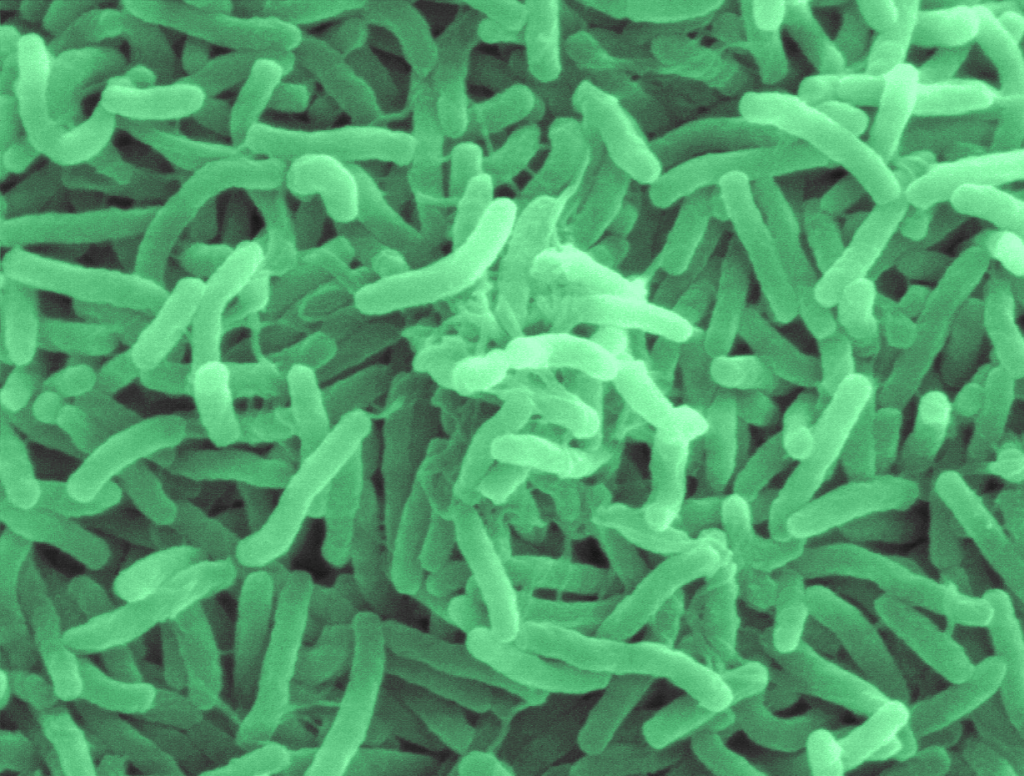
Characterised by watery diarrhoea and dehydration, cholera is caused by infection by the bacterium Vibrio cholerae and in some cases can cause death within hours. It is spread through contaminated water, and asymptomatic individuals can contribute to the spread by shedding bacteria in faeces for seven to 14 weeks.
The National Institute for Communicable Diseases (NICD) says that treatment is with oral rehydration solution (ORS), with intravenous ringer’s lactate for severe dehydration and antibiotics recommended in hospitalised patients.
For acute cases of watery diarrhoea, the National Institute for Communicable Diseases (NICD) advises the following course of action:
– Collect a stool or rectal swab specimen and request culture for cholera (in addition to other microbiological tests etc. as indicated). Where possible, collect specimens before antibiotic treatment is given. Guidance on the collection of specimens can be found here (https://www.nicd.ac.za/wp-content/uploads/2023/01/Guidelines-for-specimen-collection-Cholera-Janury2023.pdf)
– Notify the case as suspected cholera by completing a Notifiable Medical Conditions case notification form. Do this immediately; don’t wait for laboratory results.
For management of suspected cholera cases, NICD provides the following guidance:
Rehydration is the mainstay of treatment.
1. Assess and reassess the degree of dehydration frequently.
2. Replace fluid and maintain hydration status based on the degree of dehydration (see flowchart)
3. Antibiotic therapy is recommended for hospitalised patients. Ciprofloxacin is currently the antibiotic of choice:
Paediatric dose: 20 mg/kg (max 1g) po stat
Adult dose: 1g po stat
4. Children < 5 years of age should be given zinc supplementation.
5. Patients should be fed as soon as they can tolerate food
6. Patients who are no longer dehydrated and can take ORS and have decreased frequency of diarrhoea may be discharged.
7. Don’t prescribe anti-motility drugs (eg loperamide)
8. Isolate patient if possible and apply contact precautions
The guidance also covers laboratory sampling and infection control procedures. Further resources are available on their website.

