Inhibitor Drugs to Treat Aggressive Breast Cancer Identified
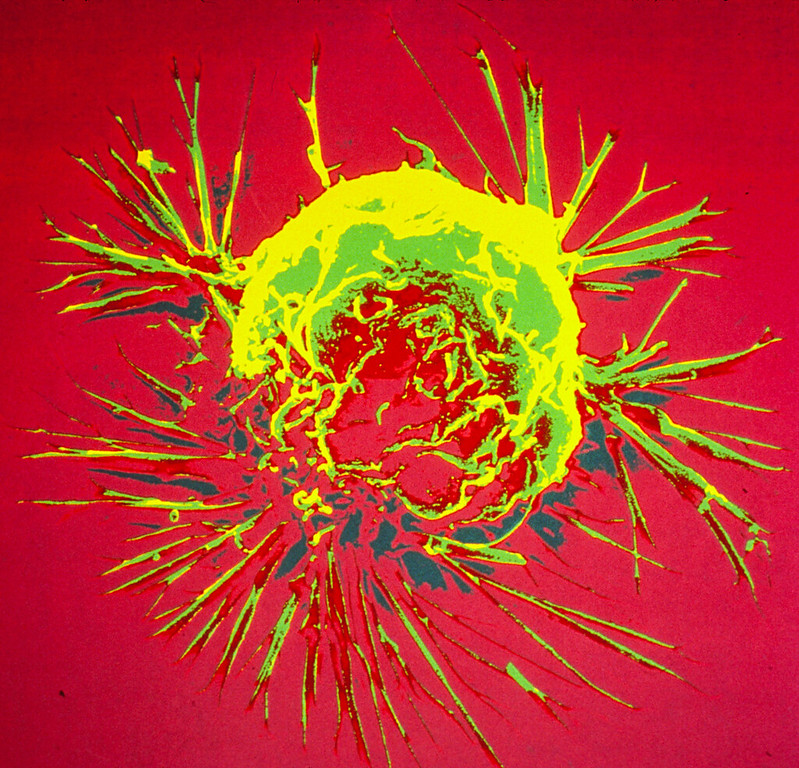
A US study seeking more effective treatment for deadly metaplastic breast cancer has identified two inhibitor drugs with the potential to interrupt disease progression.
Houston Methodist and a team of researchers from across the country examined the biology of metaplastic breast cancer, comparing it to non-metaplastic triple negative breast cancer. They discovered metaplastic breast cancers typically exhibit two unique signaling pathways in their cell interaction. Researchers were able to disrupt these pathways using a class of inhibitors typically used to treat advanced cancers – phosphoinositide 3 kinase inhibitor (P13K) – in combination with a nitric oxide inhibitor (NOS) typically used to treat septic shock, cardiovascular disease and other conditions. When introduced to the cell, these drugs disrupted these pathways, making the treatment more effective.
A rare and aggressive form of disease, metaplastic breast cancer typically grows faster and is more likely to metastasise than other breast cancers. It is also more likely to recur after successful initial treatment. Patients with metaplastic breast cancer will often receive the same treatment as a patient with triple negative breast cancer, another aggressive and deadly form of the disease. However, metaplastic breast cancer often does not respond well.
The findings are published in Nature Communications The study’s corresponding author is Dr Jenny Chang, the executive vice president, president and CEO, and chief academic officer at the Houston Methodist Academic Institute.
“This is a significant finding because it offers a promising therapeutic option for one of the most aggressive and difficult-to-treat subtypes of breast cancer,” said Chang. “We have the potential to improve outcomes for patients who currently face limited treatment options and poor prognoses, marking an important step forward in cancer research and therapy.”
The first author, Dr Tejaswini Reddy, hopes these findings will help develop a specific care plan for metaplastic cancer patients and improve long-term survival of the disease.
“Our findings highlight a promising therapeutic combination that could hopefully change the landscape of metaplastic breast cancer treatment. Translating this research into a National Cancer Institute-funded clinical trial is crucial to improving outcomes for patients facing this rare and aggressive disease. Moreover, this approach may have broader implications, potentially benefiting patients with other cancers with similar biology,” said Reddy.
The findings of this preclinical study have translated into a National Cancer Institute (NCI)-funded phase 2 clinical trial to help patients with this rare and aggressive malignancy (https://clinicaltrials.gov/study/NCT05660083).
Source: Houston Methodist





