The Spread of a Highly Drug-resistant Cholera Strain
Scientists from the National Reference Center for Vibrios and Cholera at the Institut Pasteur, in collaboration with the Centre hospitalier de Mayotte, have revealed the spread of a highly drug-resistant cholera strain from Yemen down through Africa. The study was published in the New England Journal of Medicine.
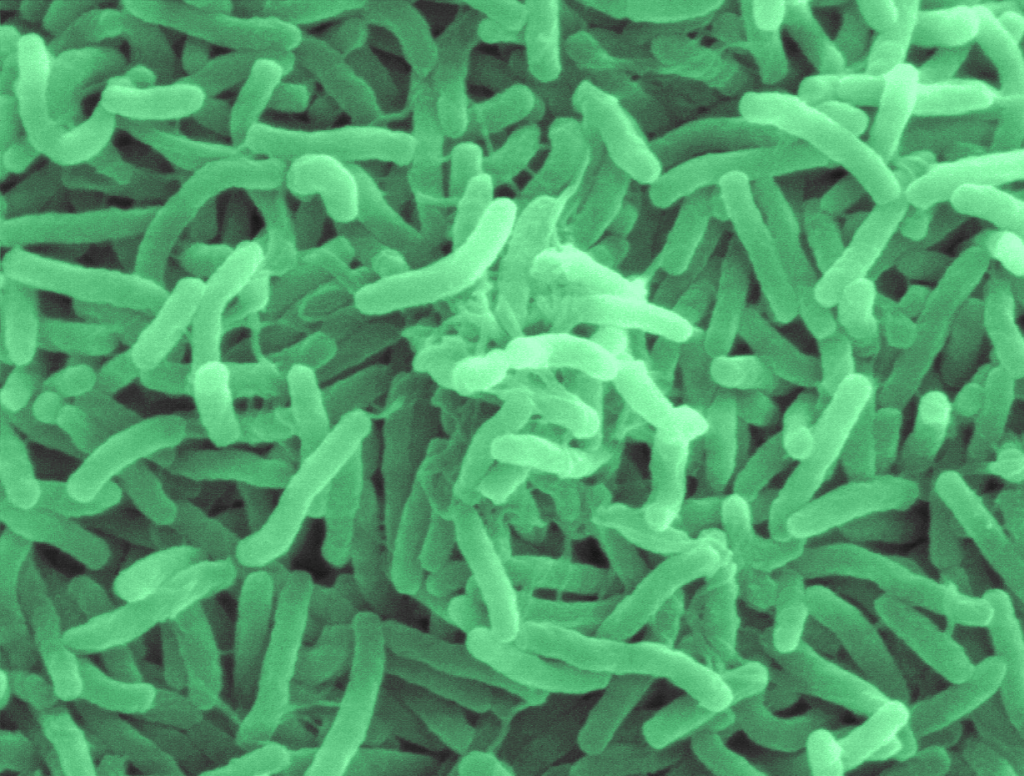
Cholera is caused by the bacteria Vibrio cholerae and in its most severe forms, it is one of the most rapidly fatal infectious diseases: in the absence of treatment, patients can die within hours. Treatment primarily involves replacing lost water and electrolytes, but antibiotics are also used in addition to rehydration therapy. They are essential in reducing the duration of infection and breaking chains of transmission as quickly as possible.
A strain resistant to ten antibiotics – including azithromycin and ciprofloxacin, two of the three recommended for treating cholera – was identified for the first time in Yemen during the cholera outbreak in 2018-2019[1].
Scientists have now been able to trace the spread of this strain by studying the bacterial genomes. After Yemen, it was identified again in Lebanon in 2022[2], then in Kenya in 2023, and finally in Tanzania and the Comoros Islands – including Mayotte, a French département off the south-east coast of Africa – in 2024. Between March and July 2024, the island of Mayotte was affected by an outbreak of 221 cases caused by this highly drug-resistant strain.
“This study demonstrates the need to strengthen global surveillance of the cholera agent, and especially to determine how it reacts to antibiotics in real time. If the new strain that is currently circulating acquires additional resistance to tetracycline, this would compromise all possible oral antibiotic treatment,” concludes Professor François-Xavier Weill, Head of the Vibrios CNR at the Institut Pasteur and lead author of the study.
[1] Press release 19/08/2023 – Genes fuelling antibiotic resistance in Yemen cholera outbreak uncovered
[2] https://www.nature.com/articles/s41467-024-51428-0
Source: Institut Pasteur



