The High Cost of Having Too Few Pharmacists in SA

By Chris Bateman
It’s acknowledged in key policy documents, well known at the coalface and much ventilated in the media: South Africa’s public healthcare system has too few healthcare workers, especially medical doctors, certain specialists, and theatre nurses. Less recognised however is the shortage of public sector pharmacists. We lift the lid on this until now largely hidden problem – and its impact.
There are too few public sector pharmacy posts across South Africa to deliver a comprehensive service, with no clear staffing norms, and an uneven distribution of pharmacists, especially in rural districts. This contributes in part to medicine stockouts and the emergence of deadly hospital-acquired drug-resistant infections.
This is according to Dr Andy Gray, a senior lecturer in the Division of Pharmacology at the University of KwaZulu-Natal’s School of Health Sciences and co-head of the World Health Organization Collaborating Centre for Pharmaceutical Policy and Evidence Based Practice. His views are echoed by at least two other key local stakeholder organisations.
Flagging the alarming rise in resistance to antimicrobials – an urgent global public health threat – driven by the misuse of antibiotics in hospitals and ambulatory care, Gray told Spotlight that there are not enough pharmacists to intervene if they see inappropriate use of medicines.
“This just continues without any effort to fix it. Inadequately trained and understaffed prescribers are working under immense stress, so they are prone to use the wrong medicines at the wrong time with the wrong doses,” he said. “There are also very few microbiologists and certainly not enough pharmacists at the bedside. They’re not doing what’s necessary to ensure the proper use of medicines – for example, better control over antimicrobials.”
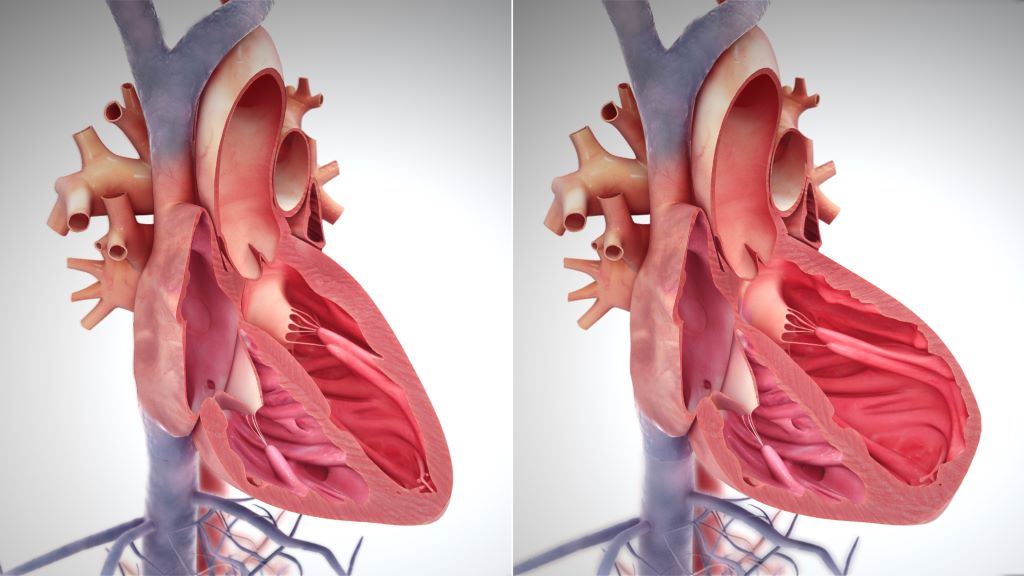
The excessive dependence on antibiotics has resulted in the emergence of antibiotic-resistant bacteria, commonly known as superbugs. This is called bacterial resistance or antibiotic resistance. Some bacteria are now resistant to even the most powerful antibiotics available.
South Africa has been ranked 67th out of 204 countries for deaths – adjusted by age per 100 000 people – linked to antimicrobial resistance. It has been estimated that around 9 500 deaths in the country in 2019 were directly caused by antimicrobial resistance, while 39 000 deaths were possibly related to resistant infections.
The National Department of Health warned in a background document that rising antimicrobial resistance and the slow-down of new antibiotics could make it impossible to treat common infections effectively. This could also lead to an increase in the cost of healthcare because of the need for more expensive 2nd or 3rd line antimicrobial agents, as well as a reduced quality of life.
Low numbers
Gray said that while not matching the paucity of public sector doctors and nurses, pharmacists stand at 24% of the staffing levels calculated as necessary to deliver a comprehensive service.
“We need just over 50 pharmacists per 100 000 uninsured population as a target, but we’re sitting at around 12,” he said.
Gray said the SA Pharmacy Council (SAPC) has no data on the total number of pharmacists actually working in the country, or the number working in particular settings. A SAPC spokesperson said they had only provincial statistics, but could not track pharmacist movements.
“You can’t use their database to find out how many pharmacists are working where. The Health Systems Trust SA Health Review Indicator chapter has figures of public sector pharmacists per province and per 100 000 uninsured population,” Gray pointed out.
As at February 2024, there were 16 856 pharmacists registered in South Africa, (working and not working), excluding the 971 community service pharmacists.
The 5 958 pharmacists employed in the public sector represents the full complement of funded posts, but it is well below the number needed – and varies dramatically between provinces. While almost all funded posts are filled, Gray said the number of posts is less than needed to deliver a comprehensive, quality service.
Taken across South Africa’s population of around 62 million, there are around 28 registered pharmacists (working or not working), per 100 000 people (insured and uninsured). According to data from 2016, the mean global ratio stands at 73 per 100 000.
“We’re better than many other African countries, but that’s cold comfort,” said Gray.
Increases spread unevenly
There are some positives. The number of pharmacists in the public sector has grown since 2009, rising from five to 12 per 100 000 uninsured people by 2023. However, the ratio varies markedly by district – for example: from 15 in the best-served Western Cape district to a mere three in the poorest served Northern Cape district.
Gray said the more rural districts suffer the most when it comes to understaffing of pharmacists and this contributes to medicine stockouts. While the causes of medicine stockouts are complex, one of the major contributors is the refusal of suppliers to deliver any more stock until accounts are paid.
Understaffing of pharmacists often results in nurses managing patients without any pharmaceutical oversight, Pharmaceutical Society of South Africa Executive Director, Refiloe Mogale, told Spotlight. She associates such task-shifting with medicine misuse and inappropriate prescribing, noting that while it’s a vital strategy in budget-tight environments, medication errors are on the rise. This, she argues, could be solved by ensuring appropriate pharmaceutical personnel are placed to support primary healthcare facilities – such as pharmacist assistants.
“A Primary Care Drug Therapy (PCDT) trained pharmacist can diagnose, treat, and dispense medications. So, this is not as much about task-shifting as about the pharmacist providing comprehensive care. These PCDT pharmacists can do family planning, screening for diabetes, hypertension, and other clinical tasks that take the burden off doctors. We need more of them,” she said.
‘No clear staffing norm’
Addressing the human resources quandary, Gray said the core problem had always been that the number of pharmacist posts per hospital or clinic were not evenly distributed. “There’s been no clear staffing norm. The old ‘homeland’ hospitals are likely to be under resourced with pharmacists and pharmacists’ assistants. Posts are poorly distributed and by global standards, we’re nowhere near where we should be,” he said.
The National Department of Health’s most senior pharmacy official Khadija Jamaloodien agreed that pharmacy posts should be distributed better. But she said work protocols dictate that state pharmacists must visit each clinic in their district at least once per month. She said there are 3 000 primary healthcare facilities in the country and 6 000 (albeit maldistributed) public sector pharmacists.
Nhlanhla Mafarafara, President of the SA Association of Hospital and Institutional Pharmacists, told Spotlight too many of the almost 6 000 pharmacists in the public sector are doing stock management, dispensing, administration and management work in hospitals and pharmaceutical depots. He says the numbers do not necessarily reflect pharmacists in clinical or patient facing areas.
“The reality is that pharmacists are restricted to trying to get drug stock in and out,” Gray observed.
However, the lack of pharmacists and pharmacist assistants at clinics and hospitals means timely and/or knowledgeable ordering often results in shortages of essential medicines, something all experts interviewed for this article agreed on.
Mafarafara said that by defining what services a pharmacist should render and what’s needed to enable a quality service, more realistic staffing numbers could be reached. Pharmacies are central points in all hospitals, with closure for even an hour crippling a hospital. Thus, adequate staffing is critical to ensure uninterrupted access to good quality pharmaceutical care.
South Africa, Mafarafara added, was far behind many other countries in the effective use of pharmacists’ clinical expertise in leading evidence-based care in hospitals. “I’d even go so far as to say doctors should be stopped from dispensing in favour of pharmacists to improve quality of patient care,” he said.
‘If you don’t have a pharmacist, nothing gets done properly’
Jamaloodien said the cost of having too few pharmacists is more far-reaching than just antimicrobial resistance. “You can have stock outs because there’s nobody to manage the supply chain. In my experience, if you don’t have a pharmacist, nothing gets done properly,” she said.
Her solutions? Compliance with the “comprehensive and robust” evidence-based standard treatment guidelines, access to an updated and well-maintained cell phone-based application that gives everybody access to the latest information and medicine changes – and more attendance by all healthcare professionals of webinars held after every medicine’s committee meeting, plus clinicians regularly reading drug update bulletins to keep up with new medicines.
Republished from Spotlight under a Creative Commons licence.
Read the original article