Ignore Antifungal Resistance at Your Peril, Scientists Warn
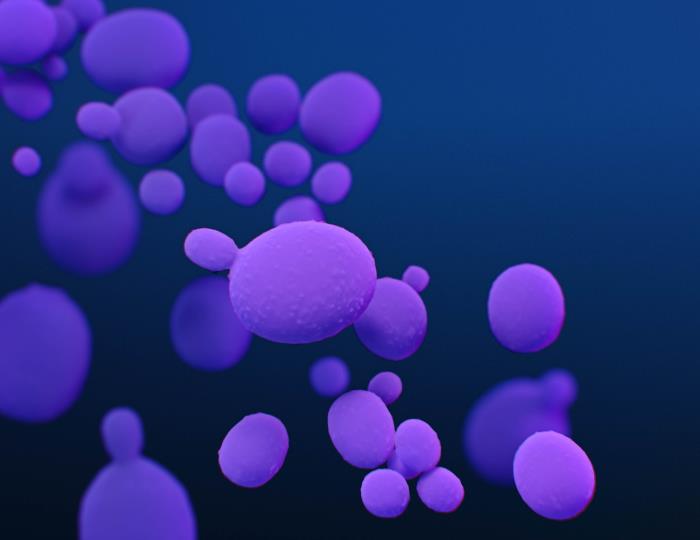
Without immediate action, humanity will potentially face further escalation in resistance in fungal disease, a renowned group of scientists from the across the world has warned. The commentary – published in ‘The Lancet’ this week – was coordinated by scientists at The University of Manchester, the Westerdijk Institute and the University of Amsterdam. According to the scientists most fungal pathogens identified by the World Health Organization – accounting for around 3.8 million deaths a year – are either already resistant or rapidly acquiring resistance to antifungal drugs.
The authors argue that the currently narrow focus on bacteria will not fully combat antimicrobial resistance (AMR). September’s United Nations meeting on antimicrobial resistance (AMR) must, they demand, include resistance developed in many fungal pathogens.
Devastating health impacts
Resistance is nowadays the rule rather than the exception for the four currently available antifungal classes, making it difficult – if not impossible – to treat many invasive fungal infections. Fungicide resistant infections include Aspergillus, Candida, Nakaseomyces glabratus, and Trichophyton indotineae, all of which can have devastating health impacts on older or immunocompromised people.
Dr Norman van Rhijn from The University of Manchester coordinated the comment with Professor Ferry Hagen from the University of Amsterdam and the Westerdijk Institute in the Netherlands.
Dr van Rhijn said: “Most people agree that resistant bacterial infections constitute a significant part of the AMR problem. However many drug resistance problems over the past decades have also been the result of invasive fungal diseases largely underrecognized by scientists, governments, clinicians and pharmaceutical companies. The threat of fungal pathogens and antifungal resistance, even though it is a growing global issue, is being left out of the debate.”
Unlike bacteria, the close similarities between fungal and human cells which, say the experts, means it is hard to find treatments that selectively inhibit fungi with minimal toxicity to patients.
Back to square one
Professor Ferry Hagen added: “Despite the huge difficulties in developing them, several promising new agents including entirely new classes of molecules, have entered clinical trials in recent years. But even before they reach the market after years of development, fungicides with similar modes of action are developed by the agrochemical industry resulting in cross-resistance. That sets us back to square one again. It is true many essential crops are affected by fungi, so antifungal protection is required for food security. But the question is, at what price?”
The scientists recommend:
- Worldwide agreement on restricting the use of certain classes of antifungal molecules for specific applications.
- Collaboration on solutions and regulations that ensure food security and universal health for animals, plants, and humans.
- Adding priority to AMR to fungal infections at the UN’s meeting in September.
Source: Universiteit van Amsterdam