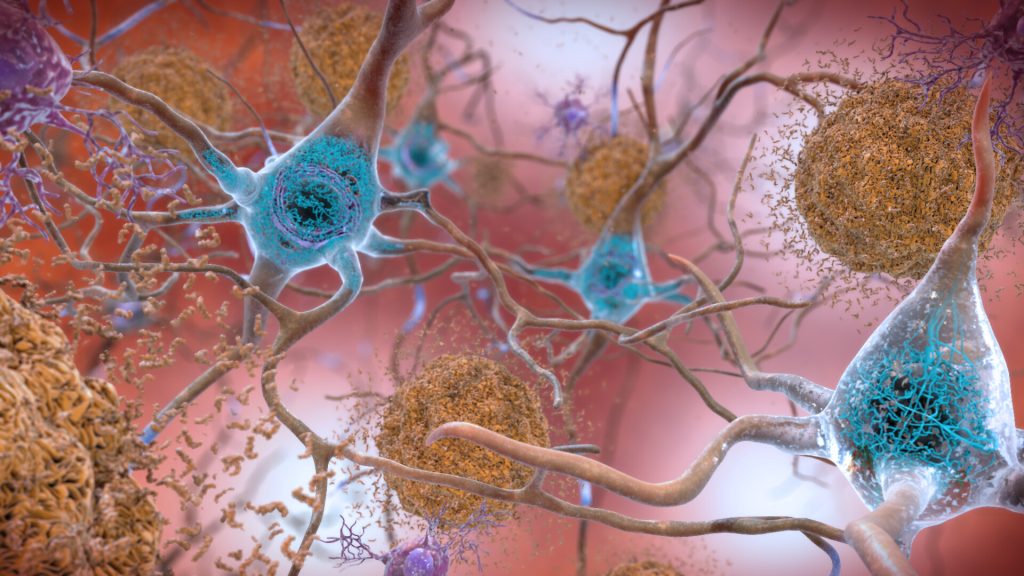
A new study by investigators from Mass General Brigham suggests that whether a person inherits risk of Alzheimer’s disease from their mother or father influences risk of biological changes in the brain that lead to disease. By evaluating 4400 cognitively unimpaired adults ages 65–85, the team found those with a history of Alzheimer’s disease (AD) on either their mother’s side or both parents’ sides had increased amyloid in their brains. Their results are published in JAMA Neurology.
“Our study found if participants had a family history on their mother’s side, a higher amyloid level was observed,” said senior corresponding author Hyun-Sik Yang, MD, a neurologist at Mass General Brigham.
Yang said that previous smaller studies have investigated the role family history plays in Alzheimer’s disease. Some of those studies suggested maternal history represented a higher risk of developing Alzheimer’s, but the group wanted to revisit the question with cognitively normal participants and access to a larger clinical trial data set.
The team examined the family history of older adults from the Anti-Amyloid Treatment in Asymptomatic Alzheimer’s (A4) study, a randomized clinical trial aimed at AD prevention. Participants were asked about memory loss symptom onset of their parents. Researchers also asked if their parents were ever formally diagnosed or if there was autopsy confirmation of Alzheimer’s disease.
“Some people decide not to pursue a formal diagnosis and attribute memory loss to age, so we focused on a memory loss and dementia phenotype,” Yang said.
Researchers then compared those answers and measured amyloid in participants. They found maternal history of memory impairment at all ages and paternal history of early-onset memory impairment was associated with higher amyloid levels in the asymptomatic study participants. Researchers observed that having only a paternal history of late-onset memory impairment was not associated with higher amyloid levels.
“If your father had early onset symptoms, that is associated with elevated levels in the offspring,” said Mabel Seto, PhD, first author and a postdoctoral research fellow in the Department of Neurology at the Brigham. “However, it doesn’t matter when your mother started developing symptoms – if she did at all, it’s associated with elevated amyloid.”
Seto works on other projects related to sex differences in neurology. She said the results of the study are fascinating because Alzheimer’s tends to be more prevalent in women. “It’s really interesting from a genetic perspective to see one sex contributing something the other sex isn’t,” Seto said. She also noted the findings were not affected by whether study participants were biologically male or female.
Yang noted one limitation of the study is some participants’ parents died young, before they could potentially develop symptoms of cognitive impairment. He said social factors like access to resources and education may have also played a role in when someone acknowledged cognitive impairment and if they were ever formally diagnosed.
“It’s also important to note a majority of these participants are non-Hispanic white,” Seto added. “We might not see the same effect in other races and ethnicities.”
Seto said the next steps are to expand the study to look at other groups and examine how parental history affects cognitive decline and amyloid accumulation over time and why DNA from the mother plays a role.
Reisa Sperling, MD, a co-author on the paper, principal investigator of the A4 Study and a neurologist at Mass General Brigham, said the findings could be used soon in clinical translation.
“This work indicates that maternal inheritance of Alzheimer’s disease may be an important factor in identifying asymptomatic individuals for ongoing and future prevention trials,” Sperling said.
Source: Mass General Brigham

