Slow Progress after Decision to Make TB Prevention Pills More Widely Available

By Tiyese Jeranji
Besides preventing illness and death, tuberculosis prevention therapy is estimated to be highly cost effective. Yet, uptake of the medication is not what it could be in South Africa. Tiyese Jeranji asks how much has changed since the Department of Health last year decided to make TB prevention therapy much more widely available.
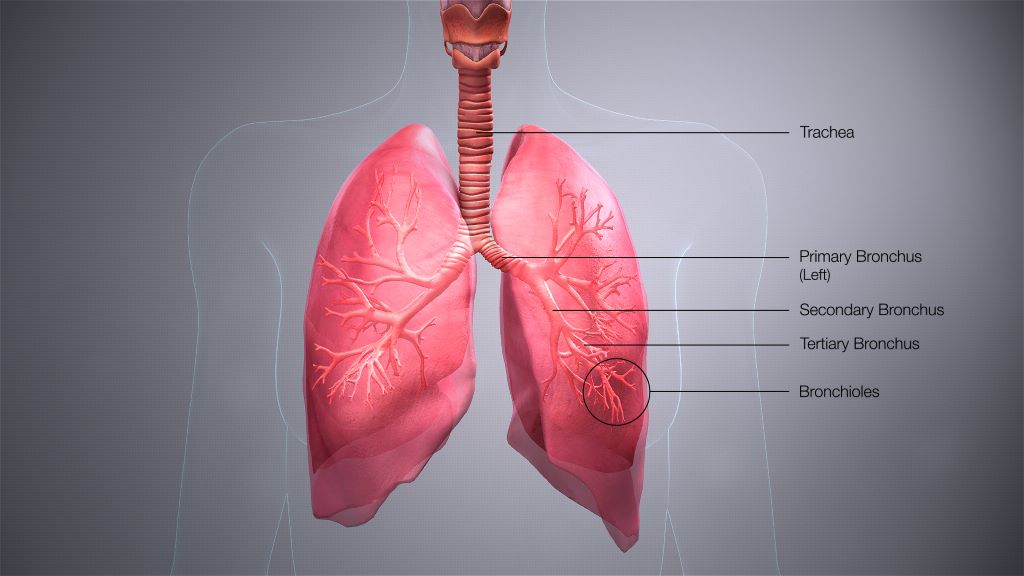
Many people who have the TB bug in their lungs are not ill with TB disease. Having the bug in your body, does mean however that you are at risk of falling ill, should the TB bacteria get the overhand in its battle with your immune system.
Fortunately, we have medications that can kill TB bacteria before one falls ill. A recent World Health Organization (WHO) investment case, suggests such TB prevention therapy, commonly called TPT, reduces the risk of falling ill with TB in those exposed to the bug by 60% to 90% compared to people who do not get the treatment.
In South Africa, TPT has been available in the public sector for years, but until the publication of new government guidelines last year, only kids aged five or younger and people living with HIV could get the medication. Under the new guidelines, everyone who has had close contact with someone with TB should be offered a TB test and if they test negative be offered TPT – if they test positive they should be offered TB treatment. These changes dramatically expanded the number of people in South Africa who are eligible for TPT.
The antibiotics used for TPT has also changed in recent years. For many years, the only option was a medication called isoniazid taken for six or more months. We now also have two three-month options – isoniazid and rifapentine given once weekly and rifampicin and isoniazid given daily. These shorter duration treatment courses should help more people complete the treatment.
Down and up?
Dr Norbert Ndjeka, Chief Director of TB Control and Management at the National Department of Health, tells Spotlight that in recent years, South Africa has seen a steady decline in the number of people initiated on TPT.
The decline has been substantial. In people living with HIV, initiation on TPT dropped from 454 000 in 2018 to around 241 000 in 2023. In children aged five and younger who have had contact with someone with TB, it fell from 25 357 in 2018 to 15 775 in 2023.
TPT enrolments per province for 2023
| Province | People living with HIV | Contacts < 5 Years | Contacts > 5 Years |
|---|---|---|---|
| Eastern Cape | 34 623 | 2 551 | 4 771 |
| Free State | 14 535 | 562 | 1 027 |
| Gauteng | 67 333 | 1 368 | 4 241 |
| KwaZulu-Natal | 62 362 | 3 168 | 8 519 |
| Limpopo | 15 871 | 391 | 452 |
| Mpumalanga | 25 618 | 669 | 2 006 |
| Northern Cape | 3 178 | 855 | 1 595 |
| North West | 9 433 | 596 | 1 425 |
| Western Cape | 8 532 | 5 615 | 1 278 |
| South Africa | 241 485 | 15 775 | 25 314 |
| *Typically, provinces with higher numbers of people diagnosed with TB or those with high numbers of people living with HIV will report higher TPT initiations. | |||
There are two significant reasons for this decline, according to Ndjeka. Firstly, declining TB incidence, and secondly, declining HIV incidence.
“With fewer people diagnosed with TB disease, fewer contacts will need TPT, and with fewer people being diagnosed with HIV, fewer people will initiate TPT regardless of TB exposure,” he says.
WHO figures have shown a significant downward trend in the estimated TB cases per year in South Africa and according to Thembisa, the leading mathematical model of HIV in South Africa, the number of people newly starting HIV treatment has dropped from a peak of over 700 000 in 2011, to well under 300 000 in 2023.
But the recent downward trend in people taking TPT may be coming to an end. “We believe that the implementation of the new guidelines within the current strategic framework will lead to increases in TPT enrolment,” says Ndjeka.
In line with the new guidelines, there are also changes to what TPT data is being collected. “For example, we never used to report on TPT provision to contacts 5 years and older, but now we do and in 2023 at least 25 314 TB contacts 5 years and older were initiated on TPT,” he says.
20% increase expected in 2024
Based on the data reported for January and February of this year, Ndjeka expects that overall TPT initiations will increase by at least 20% in 2024 compared to 2023. Moreover, as documented in the National Strategic Plan for HIV, TB and STIs 2023-2028, there is a plan to have a steady annual increase in TPT enrolments leading up to 2028.
Ndjeka says based on the NSP TPT targets, South Africa is exceeding TPT targets for people living with HIV, but reaching less than 25% of targets for TB contacts. He points out that performance varies by province, but that all provinces have a long way to go in terms of reaching TB contacts.
‘Cost saving over time’
“The aim of offering TPT is to reduce the TB incidence,” Ndjeka says. “So, if everyone eligible is offered TPT there will obviously be increased costs initially but cost saving over time. This looks at cost of treating people with TB, lives saved/ deaths prevented as well as costs to patients.”
For South Africa, he says, it is estimated that we can reduce the number of people with TB by 138 000 by 2050 at an estimated cost of R23 226.90 per TB episode prevented.
Ndjeka says it costs the health department an estimated at R1 498.51 to treat one person with drug-susceptible TB for 6 months and R16 612.82 to treat one person with the standard drug-resistant TB treatment for 6 months. “These costs are for medications alone, which can also go beyond R70 000 depending on the patient and the type of resistant TB. Moreover, when factoring in clinical consultations, hospitalisations, and costs to patients the costs go up considerably,” he says.
The cost of providing TPT also depends on the regimen. One person on TPT can cost as little as R608.77 for a course of three months of isoniazid and rifapentine given once weekly, and up to R1 358.02 for 12 months of isoniazid. “TPT also has much lower associated costs for example there is no hospitalisation, fewer clinic visits and consultations,” Ndjeka says.
“By preventing TB, the cost of TB treatment is avoided along with the costs of treating some of the acute and chronic conditions that someone with TB may experience even after being cured of TB. These include chronic obstructive pulmonary disease, bronchiectasis and pneumonia,” says Alison Best, communication manager at Cape Town-based NGO TB HIV Care.
“For children under five in particular, who are at increased risk of disseminated TB like TB meningitis, the cost of not preventing TB could be death or severe lifelong disability,” she says, adding that preventing TB in a single individual also prevents the costs associated with any onwards transmission of TB from that individual to others.
Questions over implementation
Expanded TPT eligibility has been widely welcomed, but questions have been raised over how well the new guidelines are being implemented.
Best says government austerity measures have made implementing new initiatives in the healthcare setting challenging.
“There is not much political will to implement the guidelines (to expand eligibility for TPT) at provincial and district levels and this has translated into the slow release of circulars, delays in training health workers, poor knowledge of the policy and its low prioritisation,” she says.
Ingrid Schoeman, Director of Advocacy and Strategy at TB Proof (a local advocacy group), says often when a national policy is released, there are delays at provincial-level in releasing circulars to enable health worker training.
“This results in these services not being available at district-level. In the Western Cape, civil society organisations, the [provincial] Department of Health, City of Cape Town and implementing partners are now all working together to support health worker training, and implementing community-led awareness campaigns so that all close TB contacts know they are eligible for TPT,” she says.
Best adds that tracking the data to show how many people are starting and completing TPT tends to be difficult. She notes there are many gaps in capturing the information. This includes, at times, the limited recording of information in patient folders by clinicians and suboptimal inputting of data by data capturers.
Ndjeka says the national department of health has been conducting training on the new guidelines with provincial and district TB and HIV programme managers, district support partners and other trainers.
“They are then responsible for training health care workers. The antiretroviral therapy guideline training also includes TPT. Webinars on the knowledge hub (an online training platform) have also conducted,” he says.
However, Ndjeka conceded that there is a lack of awareness about the value of TPT. “Additionally,” he says, “there is reluctance from clinicians to provide TPT. This result in poor demand for TPT. Treatment adherence is another problem especially for people on the long regimen (12 months)”.
Plans to address these challenges, among other things, include marketing TPT as treatment for TB infection rather than prevention, targeted communication strategies, community mobilisation, and ongoing training and mentoring of healthcare workers, says Ndjeka.
Republished from Spotlight under a Creative Commons licence.