Eosinophils, specialised immune cells, are identified by their distinctive granules that stain red when treated with an acidic reagent, eosin, which gave them their name. Eosinophils are typically rare in blood and tissues, accounting for about 3% of white blood cells. Their biological roles are poorly understood, but recent studies suggest that eosinophils are involved in regulating fat metabolism, repairing certain tissues, and helping fight different infections and cancers. Now, a new study has found that the cytokine Interleukin-5 (IL-5) acts differently on the production of eosinophils than previously believed.
In common diseases such as allergic asthma and rhinosinusitis, eosinophils are abnormally numerous in the blood and tissues, a condition known as eosinophilia. Eosinophilia is a clinical sign that aids in diagnosing these “eosinophil-associated” diseases and guides their treatment. It is known that eosinophilia is driven by increased production of eosinophils by the bone marrow. Since the 1990s, it has also been known that IL-5 is essential for eosinophilia. This led to the development and market introduction of precision therapies targeting IL-5 with monoclonal antibodies to treat severe forms of eosinophilic diseases. However, the effects of IL-5-blocking treatments on eosinophils remain poorly described.
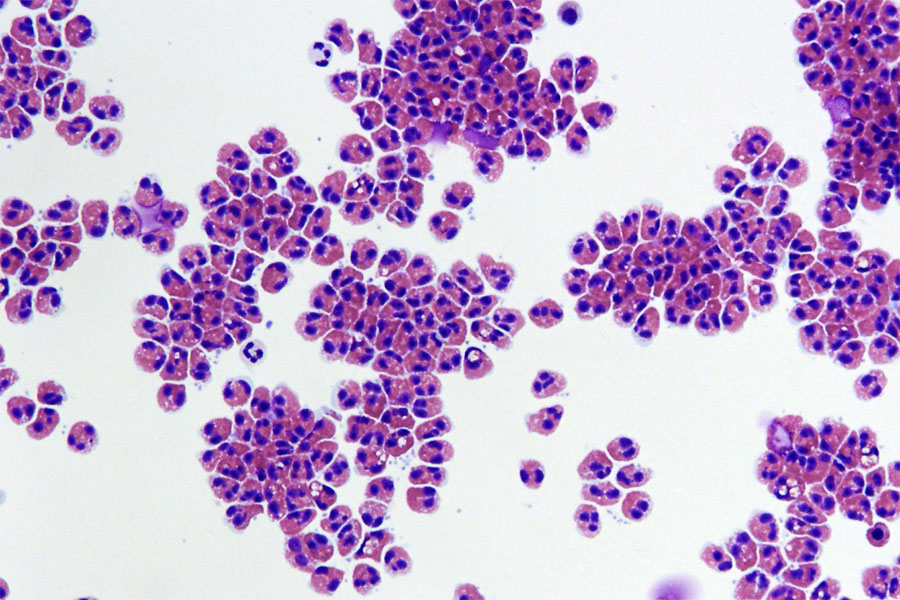
The Laboratory of Cellular and Molecular Immunology (LCMI) of the University of Liege, under the direction of Fabrice Bureau and Christophe Desmet, aimed to better understand the origin of eosinophils and eosinophilia, and the effects of treatments targeting eosinophils. As Christophe Desmet explains, “these questions previously suffered from a too rudimentary definition of the eosinophil development pathway in our bone marrow.” Two doctoral students from the laboratory, Joseph Jorssen and Glenn Van Hulst, combined their talents in bioinformatics and flow cytometry with the help of the Genomics and Flow Cytometry platforms of the GIGA Institute to finely characterise, using different approaches to analyse the surface protein and messenger RNA composition of eosinophils at various stages of their development. Although the mouse remains a reference model, collaboration with the Hematology Department of Liege University Hospital and GIGA also allowed for a very detailed and updated mapping of eosinophil development in human bone marrow, and to observe its conservation through evolution.
This detailed characterisation work, published in the journal Immunity, provides the community with simple-to-use methods and freely accessible bioinformatics data that will greatly facilitate future studies of eosinophils. Using these resources, the same study showed that IL-5 does not act as previously believed by researchers and clinicians. Most thought that IL-5 promoted the maturation of cells destined to become eosinophils and that IL-5-targeting treatments blocked this maturation. “Our study actually supports the opposite hypothesis,” explains Christophe Desmet: IL-5 slows down the maturation of developing eosinophils, allowing them to multiply longer. By stimulating this “transit amplification,” IL-5 promotes eosinophilia, and by inhibiting this process, IL-5-targeting treatments reduce it.
The researchers also showed that interferon response factor-8, considered an essential promoter of leukocyte production, was not intrinsically required for eosinophil production.
This study thus provides resources, methods, and perspectives to understand the origin of eosinophils, the effects of current precision therapies, and the regulation of eosinophil development and numbers in normal and disease conditions.
Source: University of Liège

