A rare autoimmune disease has been newly described as a COVID-related syndrome, following an investigation by the University of California San Diego School of Medicine and Leeds University.
It started when Pradipta Ghosh, MD, a professor in the Departments of Medicine and Cellular and Molecular Medicine at UC San Diego School of Medicine, received an email from Dennis McGonagle, PhD, professor of investigative rheumatology at the University of Leeds in the UK. This was the beginning of an international collaboration, one that uncovered a previously overlooked COVID-related syndrome and resulted in a paper in eBioMedicine, a journal published by The Lancet.
McGonagle asked if she was interested in collaborating on a COVID-related mystery. “He told me they were seeing mild COVID cases,” Ghosh said. “They had vaccinated around 90 percent of the Yorkshire population, but now they were seeing this very rare autoimmune disease called MDA5 – autoantibody associated dermatomyositis (DM) in patients who may or may not have contracted COVID, or even remember if they were exposed to it.”
McGonagle told of patients with severe lung scarring, some of whom presented rheumatologic symptoms – rashes, arthritis, muscle pain – that often accompany interstitial lung disease. He was curious to know if there was a connection between MDA5-positive dermatomyositis and COVID.
“DM is more common in individuals of Asian descent, particularly Japanese and Chinese,” Ghosh said. “However, Dr McGonagle was noting this explosive trend of cases in Caucasians.”
“But that’s the least of the problem,” Ghosh said. “Because he said, ‘Oh, and by the way, some of these patients are progressing rapidly to death.'”
Ghosh is the founding director of the Institute for Network Medicine at UC San Diego School of Medicine, home to the Center for Precision Computational Systems Network (PreCSN – the computational pillar within the Institute for Network Medicine). PreCSN’s signature asset is BoNE – the Boolean Network Explorer, a powerful computational framework for extracting actionable insights from any form of big-data.
“BoNE is designed to ignore factors that differentiate patients in a group while selectively identifying what is common (shared) across everybody in the group,” Ghosh explained. Previous applications of BoNE allowed Ghosh and her team to identify other COVID-related lung and heart-afflicting syndromes in adults and children, respectively.
As a rheumatologist, McGonagle specialises in inflammatory and autoimmune conditions. Ghosh said that McGonagle’s roster of patients, all within the UK’s National Health System (NHS), helped to facilitate the investigation.
“The NHS has a centralised health care database with comprehensive medical records for a large population, making it easier to access and analyse health data for research purposes,” Ghosh explained.
Ghosh and McGonagle put together a team to probe what they found was indeed an entirely new syndrome.
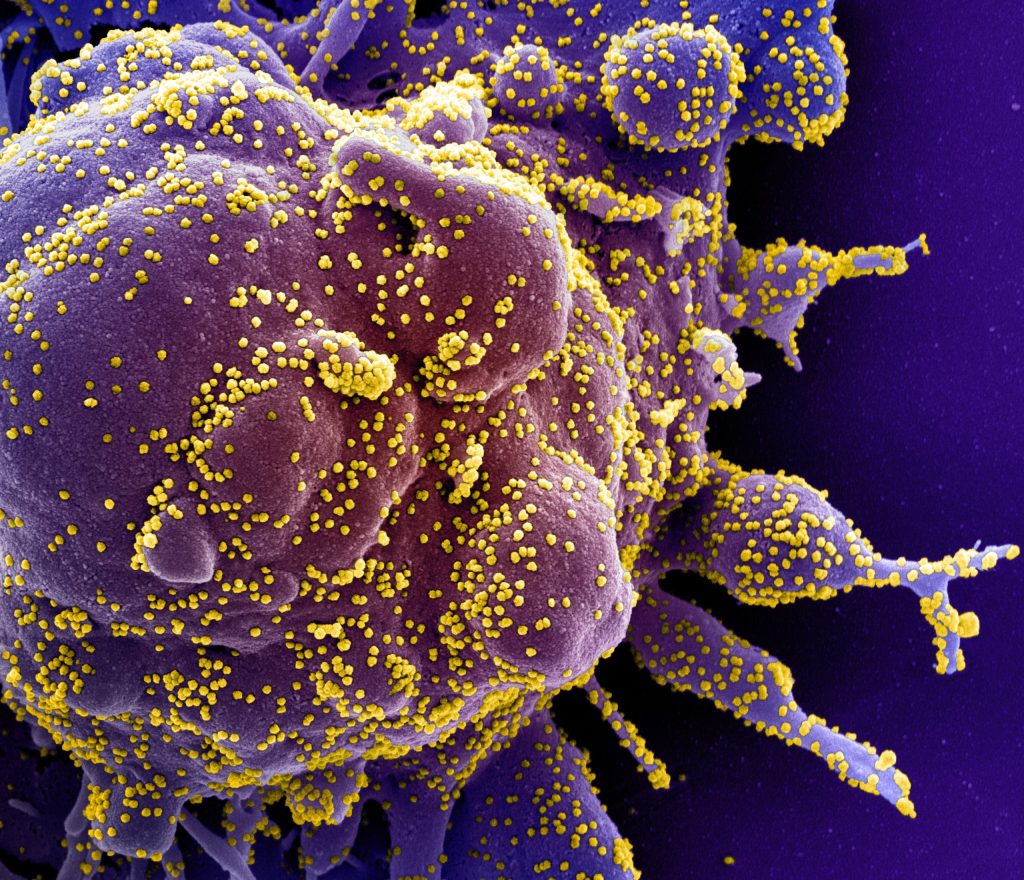
The study began with McGonagle lab’s detection of autoantibodies to MDA5 – an RNA-sensing enzyme whose functions include detecting COVID and other RNA viruses. A total of 25 patients from the group of 60 developed lung scarring, also known as interstitial lung disease. Ghosh noted that the lung scarring was bad enough to cause eight people in the group to die due to progressive fibrosis. She said that there are established clinical profiles of MDA5 autoimmune diseases.
“But this was different,” Ghosh said. “It was different in behaviour and rate of progression – and in the number of deaths.”
Ghosh and the UC San Diego team explored McGonagle’s data with BoNE. They found that the patients who showed the highest level of MDA5 response also showed high levels of interleukin-15.
“Interleukin-15 is a cytokine that can cause two major immune cell types,” she explained. “These can push cells to the brink of exhaustion and create an immunologic phenotype that is very, very often seen as a hallmark of progressive interstitial lung disease, or fibrosis of the lung.”
BoNE allowed the team to establish the cause of the Yorkshire syndrome – and pinpoint a specific single nucleotide polymorphism that is protective. By right of discovery, the group was able to give the condition a name: MDA5-autoimmunity and Interstitial Pneumonitis Contemporaneous with COVID. It’s MIP-C for short, “Pronounced ‘mipsy,'” Ghosh said, adding that the name was coined to make a connection with MIS-C, a separate COVID-related condition of children.
Ghosh said that it’s extremely unlikely that MIP-C is confined to the United Kingdom. Reports of MIP-C symptoms are coming from all over the world. She said she hopes the team’s identification of interleukin-15 as a causative link will jump start research into treatment.

