Experimental Model Identifies New Drug–drug Interactions

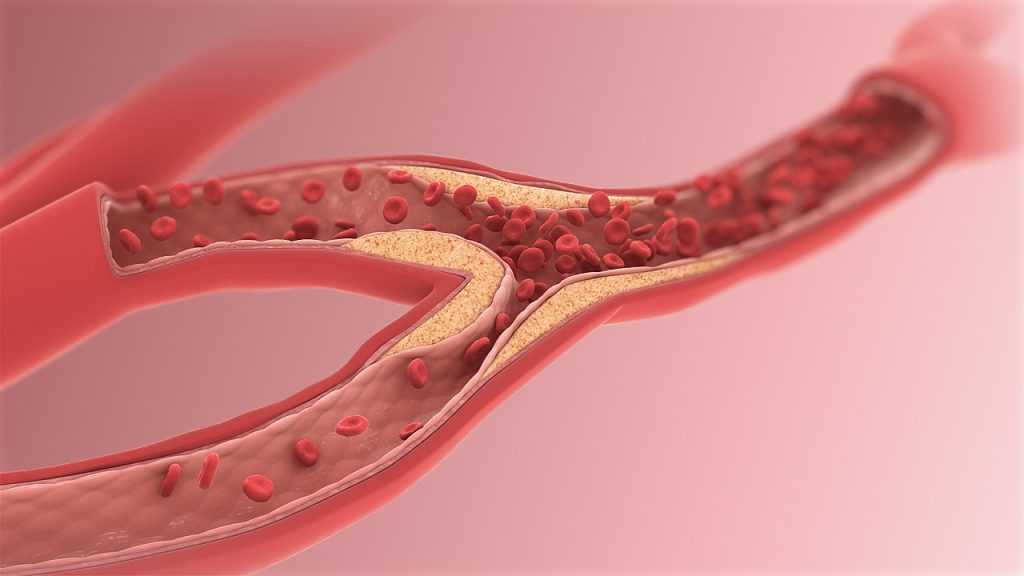
When taking oral drugs, transporter proteins found on cells that line the gastrointestinal tract facilitate their entry into the bloodstream. But for many drugs, it is not known which of those transporters they use to exit the digestive tract.
Identifying the transporters used by specific drugs could help to improve patient treatment because if two drugs rely on the same transporter, they can interfere with each other and should not be prescribed together.
Researchers at MIT, Brigham and Women’s Hospital, and Duke University have developed a multipronged strategy to identify the transporters used by different drugs, which appears in Nature Biomedical Engineering. Their approach, which makes use of both tissue models and machine-learning algorithms, has already revealed that a commonly prescribed antibiotic and a blood thinner can interfere with each other.
“One of the challenges in modelling absorption is that drugs are subject to different transporters. This study is all about how we can model those interactions, which could help us make drugs safer and more efficacious, and predict potential toxicities that may have been difficult to predict until now,” says Giovanni Traverso, an associate professor of mechanical engineering at MIT, a gastroenterologist at Brigham and Women’s Hospital, and the senior author of the study.
Learning more about which transporters help drugs pass through the digestive tract could also help drug developers improve the absorbability of new drugs by adding excipients that enhance their interactions with transporters.
Former MIT postdocs Yunhua Shi and Daniel Reker are the lead authors of the study.
Drug transport
Previous studies have identified several transporters in the GI tract that help drugs pass through the intestinal lining. Three of the most commonly used, which were the focus of the new study, are BCRP, MRP2, and PgP.
For this study, Traverso and his colleagues adapted a tissue model they had developed in 2020 to measure a given drug’s absorbability. This experimental setup, based on pig intestinal tissue grown in the laboratory, can be used to systematically expose tissue to different drug formulations and measure how well they are absorbed.
To study the role of individual transporters within the tissue, the researchers used short strands of RNA called siRNA to knock down the expression of each transporter. In each section of tissue, they knocked down different combinations of transporters, which enabled them to study how each transporter interacts with many different drugs.
“There are a few roads that drugs can take through tissue, but you don’t know which road. We can close the roads separately to figure out, if we close this road, does the drug still go through? If the answer is yes, then it’s not using that road,” Traverso says.
The researchers tested 23 commonly used drugs using this system, allowing them to identify transporters used by each of those drugs. Then, they trained a machine-learning model on that data, as well as data from several drug databases. The model learned to make predictions of which drugs would interact with which transporters, based on similarities between the chemical structures of the drugs.
Using this model, the researchers analysed a new set of 28 currently used drugs, as well as 1595 experimental drugs. This screen yielded nearly 2 million predictions of potential drug interactions. Among them was the prediction that doxycycline, an antibiotic, could interact with warfarin, a commonly prescribed blood-thinner. Doxycycline was also predicted to interact with digoxin, which is used to treat heart failure, levetiracetam, an antiseizure medication, and tacrolimus, an immunosuppressant.
Identifying interactions
To test those predictions, the researchers looked at data from about 50 patients who had been taking one of those three drugs when they were prescribed doxycycline. This data, which came from a patient database at Massachusetts General Hospital and Brigham and Women’s Hospital, showed that when doxycycline was given to patients already taking warfarin, the level of warfarin in the patients’ bloodstream went up, then went back down again after they stopped taking doxycycline.
That data also confirmed the model’s predictions that the absorption of doxycycline is affected by digoxin, levetiracetam, and tacrolimus. Only one of those drugs, tacrolimus, had been previously suspected to interact with doxycycline.
“These are drugs that are commonly used, and we are the first to predict this interaction using this accelerated in silico and in vitro model,” Traverso says. “This kind of approach gives you the ability to understand the potential safety implications of giving these drugs together.”