Trial comparing anticoagulant and antiplatelet therapy ends in a draw
Administering apaxiban to patients with cryptogenic stroke and evidence of atrial cardiopathy to prevent recurrence was no more effective than giving aspirin, a large randomised trial has found. The trial, published in JAMA, did however find a possible slight advantage in safety of apaxiban over aspirin.
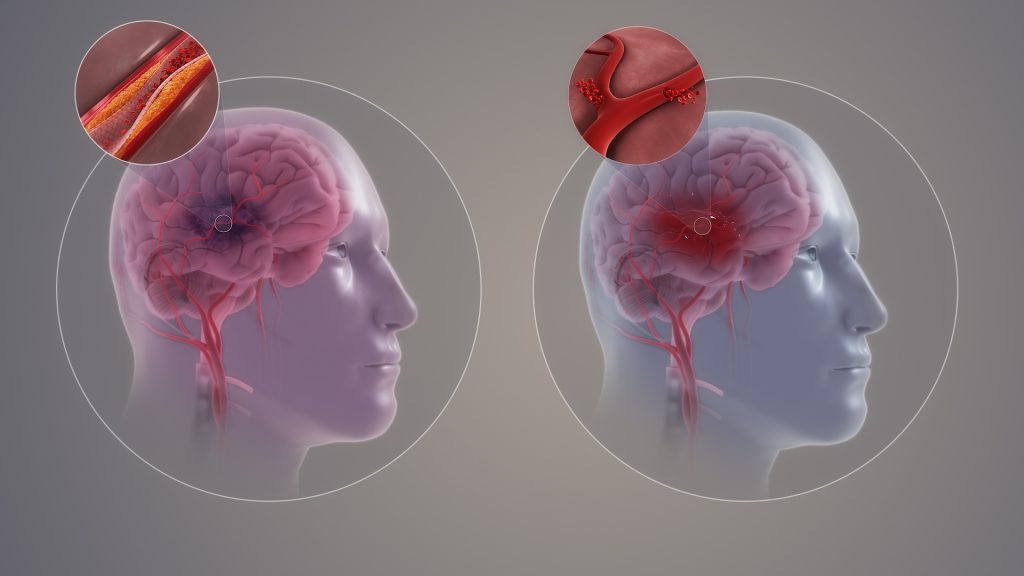
Cryptogenic stroke (CS) is cerebral ischaemia of obscure or unknown origin. One third of ischaemic strokes are cryptogenic.
Atrial cardiopathy is defined as any complex of structural, architectural, contractile, or electrophysiologic changes affecting the atria with the potential to produce clinically relevant manifestations. Atrial cardiopathy is strongly associated with incident atrial fibrillation and plays a role in thromboembolism related to atrial fibrillation.
Atrial cardiopathy is associated with stroke in the absence of clinically apparent atrial fibrillation. But it was not known whether anticoagulation, which has proven benefit in atrial fibrillation, prevents stroke in patients with atrial cardiopathy and no atrial fibrillation. The Atrial Cardiopathy and Antithrombotic Drugs in Prevention After Cryptogenic Stroke (ARCADIA) trial was therefore designed to determine whether anticoagulation is superior to antiplatelet therapy for preventing recurrent stroke in such patients.
From 2018 to 2023, the researchers conducted a multicentre, double-blind, phase 3 randomised clinical trial of 1015 participants with CS and evidence of atrial cardiopathy – defined as P-wave terminal force greater than 5000μV×ms in electrocardiogram lead V1, serum N-terminal pro-B-type natriuretic peptide level greater than 250pg/mL, or left atrial diameter index of 3cm/m2 or greater on echocardiogram. Participants had no evidence of atrial fibrillation at the time of randomisation.
The participants were randomised 1:1 to receive either apaxiban (5mg or 2.5 mg) twice daily or aspirin (81mg) once daily. The primary outcome measure of stroke occurrence was identical in both arms (40 patients, 4.4%).
There were zero intracranial haemorrhage events for apaxiban vs seven for aspirin, which is known to increase the risk of these. This supports a superior safety profile for apxiban over aspirin, but given the small number of events, the authors caution that this may be a chance finding.
Study limitations included a higher than expected dropout rate due to the COVID pandemic. Additionally, few patients met the atrial cardiopathy criterion of severe left atrial enlargement, but restricting the trial participants to this criterion would have rendered the trial infeasible.

