Destroying Tumour Cells with Calcium
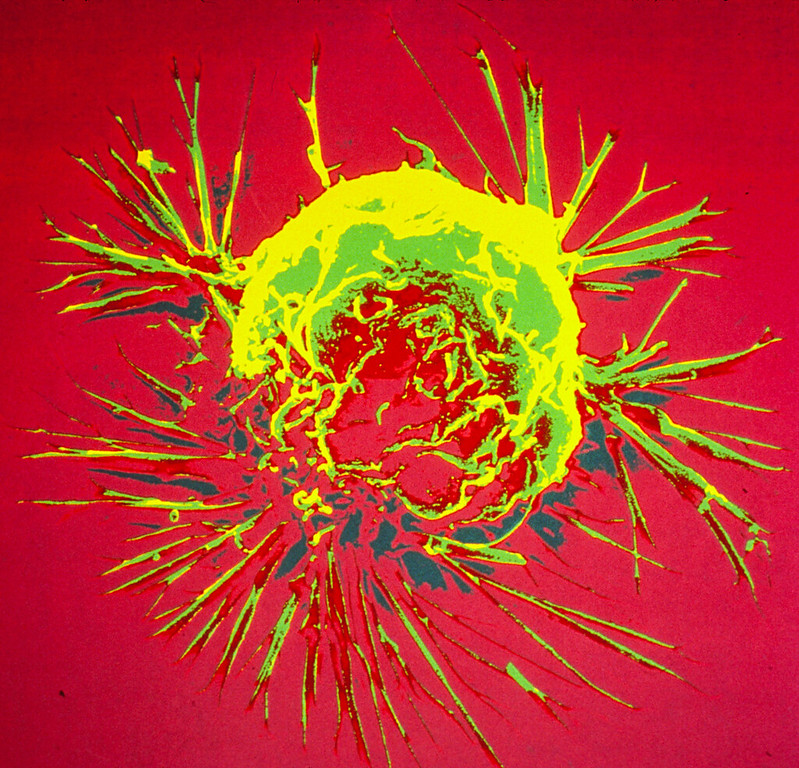
Calcium ions are essential for cells, but can be toxic in higher concentrations. A team of researchers has now designed and prepared a combination drug that kills tumour cells by modulating the calcium influx into the cell. An external calcium source is not necessary because only the calcium ions already present in the tumour tissue are used, according to the study published in the journal Angewandte Chemie.
Biological cells need calcium ions, among other things, for the proper functioning of the mitochondria, the powerhouses of the cells.
However, if there is too much calcium, the mitochondrial processes become unbalanced and the cell suffocates.
A research group led by Juyoung Yoon of Ewha Womens University in Seoul, South Korea, together with teams from China, has now taken advantage of this process and developed a synergistic antitumour drug that can open calcium channels and thus trigger a deadly calcium storm inside the tumour cell.
The researchers targeted two channels, the first one in the outer membrane, and the other was a calcium channel in the endoplasmic reticulum, a cell organelle that also stores calcium ions.
The channel located in the outer membrane opens when it is exposed to a large amount of reactive oxygen species (ROS), while the channel in the endoplasmic reticulum is activated by nitric oxide molecules.
To generate the ROS that open the outer membrane calcium channel, the researchers used the dye indocyanine green.
This bioactive agent can be activated by irradiation with near-infrared light, which not only triggers reactions that lead to ROS, but it also heats up the environment.
The team explains that the high local temperature activates the other active agent, BNN-6, to release nitric oxide molecules that open the channel in the endoplasmic reticulum.
Following successful trials in tumour cell lines, the team tested an injectable formulation in tumour-implanted mice.
To create a biocompatible combined drug, the researchers loaded the active ingredients into tiny modified porous silica beads that are not harmful to the body, but can be recognized by tumour cells and transported into the cell.
After injecting the beads into the bloodstream of the mice, the researchers observed that the drug accumulated in the tumour.
Exposure to near-infrared light successfully triggered the mechanism of action, and the tumour disappeared after a few days in mice that received the preparation.
The authors emphasise that this ion influx approach may also be useful in related biomedical research areas where a similar mechanism could activate ion channels different from calcium in order to find new therapeutic approaches.
Source: Wiley





