Syphilis had its Roots in the Americas

A research team led by members of the Max Planck Institute for Evolutionary Anthropology has taken a crucial step towards resolving a long-standing controversy – was syphilis introduced to Europe from the Americas at the end of the 15th century, or had it been there all along? Ancient pathogen genomes from skeletons that pre-date 1492 confirm its introduction from the Americas, but its world-wide spread remains a grim legacy of the colonial period.
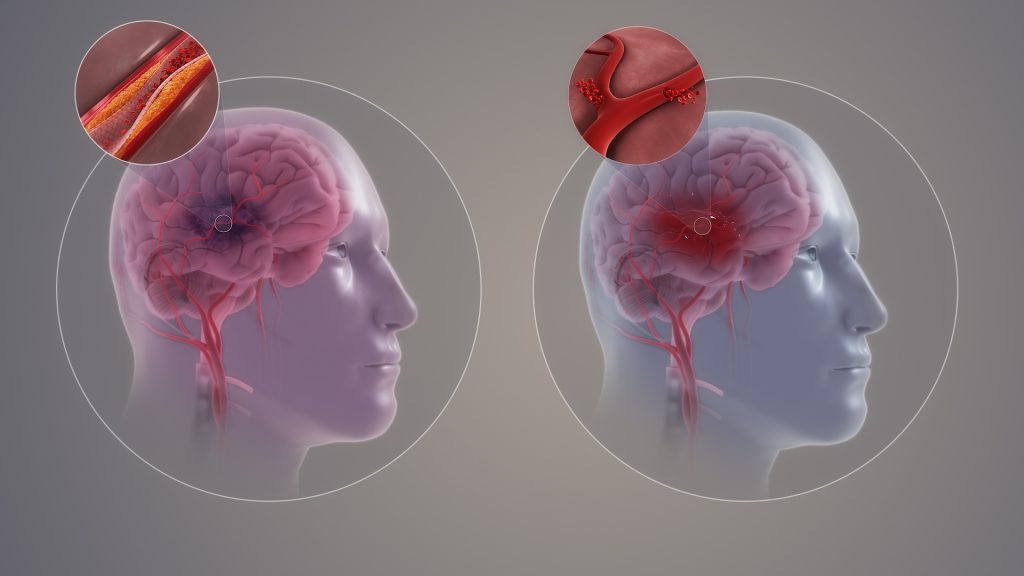
In spring 1495, the Italian campaign of Charles VIII of France was interrupted by an intense outbreak of an apparently unknown illness – a disease of high mortality that quickly engulfed the whole of Europe and left its survivors with life changing impairments to their bodies and minds. This documented epidemic is now interpreted to be the first historical account of syphilis.
The origin of syphilis is the subject of a decades-long debate. The late 15th century outbreak occurred shortly after the return of Columbus and his crew from their early expeditions to the Americas, which led some to believe that contact with new lands and people may have had something to do with the sudden disease onset. Though many communicable diseases made a westward journey from Europe to the Americas during the early colonial period where they imparted devastating consequences on indigenous groups, syphilis is one of the few that possibly made the reverse journey.
This “Columbian theory” for syphilis has gained popularity over the years, but still has its critics. Its simple narrative starts to unravel when experts turn their attention to lesions seen in bones from Mediaeval Europe. Both long-term sufferers and those born with an infection can develop changes in their bones or teeth, and over the past several decades, a number of such skeletons have been found in Europe that predate 1492. Many now believe the history of syphilis in Europe began long before Columbus, and the late 15th century pandemic happened for reasons independent of new contacts. But neither theory has been confirmed.
Analysing five ancient pathogen genomes
Pathogen DNA retrieved from archaeological bone has the potential to tip the scales in support of one theory over another. It has already told us volumes about the deep history of plague, tuberculosis, leprosy, and smallpox, though unthreading the history of syphilis has proven more challenging. “Several genomes from the syphilis family have been reconstructed from archaeological bone, but these haven’t been able to address core questions related to the pre- or post-Columbian theories surrounding syphilis”, says Kirsten Bos, group leader for molecular paleopathology at the Max Planck Institute for Evolutionary Anthropology.
A new study led by Bos and Johannes Krause, director of the Department of Archaeogenetics at the Max Planck Institute for Evolutionary Anthropology in Leipzig, has taken a critical step toward resolving this debate. Working with scientists and archaeologists from several countries in the Americas, the study focused on archaeological bone from these regions, where infections that left lesion patterns similar to syphilis are apparent from deep time periods. It is published in Nature.
“We’ve known for some time that syphilis-like infections occurred in the Americas for millennia, but from the lesions alone it’s impossible to fully characterise the disease”, comments Casey Kirkpatrick, a postdoctoral researcher and paleopathologist who contributed to the current study. Bone pathology also cannot tell us whether the disease originated in the Americas, or if it came from Asia deep in our past and merely accompanied groups during the early peopling events of the Americas some 15000 years ago.
Using state of the art techniques, the team was able to recover and analyse five ancient genomes of the syphilis disease family from Mexico, Chile, Peru, and Argentina. Computational microbiologist and postdoctoral researcher Lesley Sitter undertook the task of putting together the ancient molecular puzzles and adds “while preservation posed some analytical challenges, we were able to confidently determine the relationships between these extinct forms and the strains that impact global health today”.
Syphilis family of diseases in the Americas pre-dates “Columbus”
Syphilis is part of a small family of diseases that also includes yaws and bejel, both classified as neglected tropical diseases that are found in equatorial regions across the globe. Postdoctoral researcher Rodrigo Barquera has worked previously with archaeological bone from colonial Mexico, and has confirmed the presence of both syphilis and yaws in Mexico City by the 17th century.
Drawing upon the latest ancient genomic data, it is now clear that the Americas were a hub for ancient diversity within this disease group before the arrival of Columbus. “We see extinct sister lineages for all known forms of this disease family, which means syphilis, yaws, and bejel are the modern legacies of pathogens that once circulated in the Americas”, asserts Barquera.
“The data clearly support a root in the Americas for syphilis and its known relatives, and their introduction to Europe starting in the late 15th century is most consistent with the data”, adds Bos. Subsequent to this, an explosion in cases of syphilis and yaws seems to have occurred around AD 1500. This is likely behind the breadth and intensity of the 16th century outbreak in Europe, whose global spread was facilitated by human trafficking networks and European expansions across the Americas and Africa in the decades and centuries that followed. “While indigenous American groups harboured early forms of these diseases, Europeans were instrumental in spreading them around the world,” she concludes.
With support for an American origin of syphilis, how does the current narrative square up with the evidence of syphilis-like bone lesions that many claim to have identified in pre-1492 Europe? “The search will continue to define these earlier forms, and ancient DNA will surely be a valuable resource”, comments Krause. “Who knows what older related diseases made it around the world in humans or other animals before the syphilis family appeared.”