Public Urged To Use Registered Ozempic Products

The South African Health Products Regulatory Authority (SAHPRA) is aware of the falsified Ozempic products currently being sold on the market and online.
SAHPRA has been informed of advertisements regarding unauthorised Ozempic/semaglutide-containing products that are being disseminated through radio stations and social media platforms.
The Regulator is warning the public to be wary of products claiming to be Ozempic (semaglutide) which are not approved by SAHPRA.
Ozempic is a Schedule 4, prescription-only medicine, authorised by SAHPRA only for the treatment of type 2 diabetes mellitus in adults. SAHPRA has not authorised/registered Ozempic for weight-loss, therefore, use in that regard would be off-label. It must be noted that only a healthcare practitioner can make a Schedule 4 product available off-label as they would provide the requisite guidance and support to the patient/individual.
Novo Nordisk South Africa, who is the Holder of Certificate of Registration (HCR) has confirmed a national shortage of Ozempic stock; this resulted in limited access to treatment for diabetic patients. This may have created an opportunity for falsified/counterfeit products flooding the market claiming to be Ozempic and being used off-label for weight loss. Consumers should be wary of online offers for products claiming to be Ozempic or semaglutide.
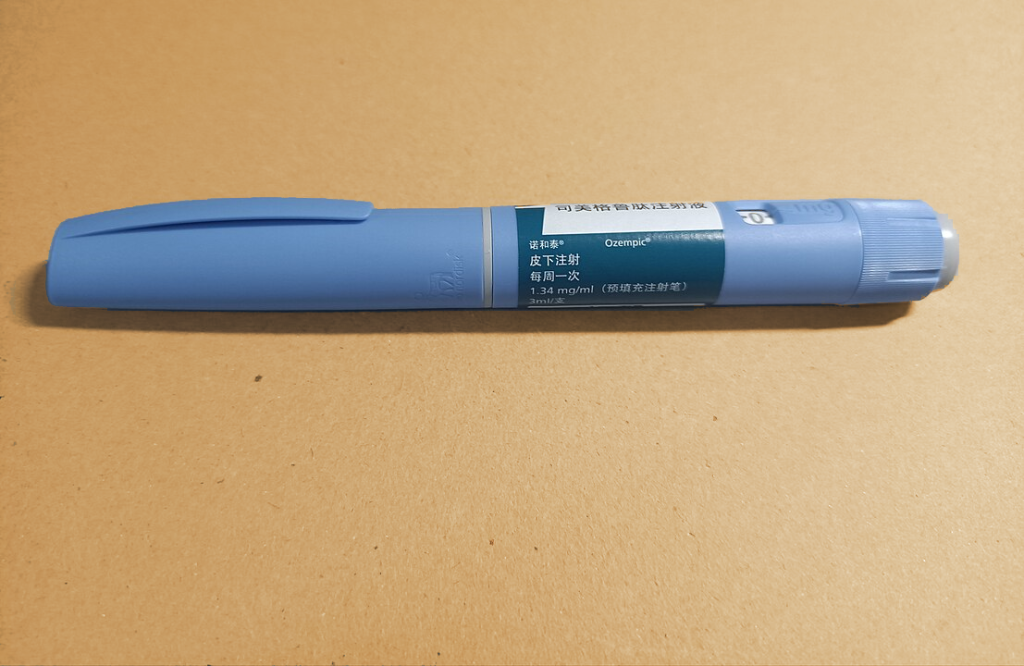
Currently, there are no generic versions of this medicine being lawfully manufactured. Therefore, any product not manufactured by Novo Nordisk claiming to contain semaglutide is likely to be fake or counterfeit. The public is being exposed to many different types of unregistered/unauthorised products that are either substandard or falsified thereby putting their health at risk. See examples of registered vs counterfeit products.
Registered products safe to use
Ozempic solution for injection is a registered product by SAHPRA belonging to the HCR, Novo Nordisk South Africa.
There are only two (2) registered presentations of the pre-filled pen for Ozempic available in South Africa namely, Ozempic 0,25 mg and 0,5 mg/dose pen and Ozempic 1 mg/dose pen.
What the public should know
- Using unregistered semaglutide products claiming to have the effects of Ozempic bought from unverified/illegally trading suppliers could be detrimental to your health as these have not been evaluated by SAHPRA for safety, quality, and efficacy.
- These falsified/fake Ozempic products may contain certain active ingredients found in the registered Ozempic products; however, the formulations or manufacturing processes may be different. These formulations have not been evaluated by SAHPRA.
- SAHPRA urges the public to first consult their medical professionals for their health treatment and prescriptions, and only purchase or use SAHPRA registered/authorised products sold at registered pharmacies.
- Any medicines that are bought outside of the legal supply chain:
- May not contain any active ingredient.
- May contain dangerous levels of the active ingredient.
- May contain another active ingredient such as insulin instead of semaglutide.
- May contain harmful inactive ingredients.
- May be nonsterile and contaminated with microbes, therefore not suitable for injection.
“Protecting the health of South Africans is top of mind for the regulator. The scourge of unregistered, substandard, and falsified medicines on the market is a serious health risk for the public. SAHPRA is listening to the public concerns, and we have an ongoing investigation into these falsified Ozempic and unregistered semaglutide-containing products”, indicates SAHPRA CEO, Dr Boitumelo Semete-Makokotlela.
Public are urged to report any suspected products that are falsely claiming to work like Ozempic. You can report through these whistle blower platforms, SAHPRA’s 24-hour hotline (0800 204 307) or via our web reporting facility: .