Moderate to severe traumatic brain injury carries lasting effects: trouble with focussing, recall and decision-making. Though many recover enough to live independently, their impairments prevent them from returning to school or work and from resuming their social lives. Current treatments offer little improvement, but results of a clinical trial of a new brain stimulation device, published in Nature Medicine, have shown great promise in at least partially restoring cognitive function.
“In general, there’s very little in the way of treatment for these patients,” said Jaimie Henderson, MD, professor of neurosurgery and co-senior author of the study.
But the fact that these patients had emerged from comas and recovered a fair amount of cognitive function suggested that the brain systems that support attention and arousal – the ability to stay awake, pay attention to a conversation, focus on a task – were relatively preserved.
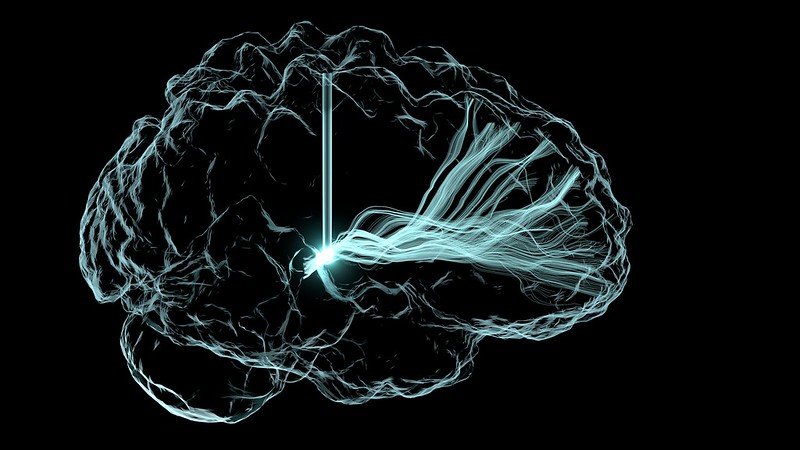
These systems connect the thalamus, a relay station deep inside the brain, to points throughout the cortex, the brain’s outer layer, which control higher cognitive functions.
‘Dimmed lights’
“In these patients, those pathways are largely intact, but everything has been down-regulated,” said Henderson, the John and Jene Blume-Robert and Ruth Halperin Professor. “It’s as if the lights had been dimmed and there just wasn’t enough electricity to turn them back up.”
In particular, an area of the thalamus called the central lateral nucleus functions as a hub that regulates many aspects of consciousness.
“The central lateral nucleus is optimised to drive things broadly, but its vulnerability is that if you have a multifocal injury, it tends to take a greater hit because a hit can come from almost anywhere in the brain,” said Nicholas Schiff, MD, a professor at Weill Cornell Medicine and co-senior author of the study.
The researchers hoped that precise electrical stimulation of the central lateral nucleus and its connections could reactivate these pathways, turning the lights back up.
Precise placement
In the trial, the researchers recruited five participants who had lasting cognitive impairments more than two years after moderate to severe traumatic brain injury. They were aged 22 to 60, with injuries sustained three to 18 years earlier.
The challenge was placing the stimulation device in a small target in the right area, which varied across individuals. Each brain is shaped differently to begin with, and the injuries had led to further modifications.
“That’s why we developed a number of tools to better define what that area was,” Henderson said. The researchers created a virtual model of each brain that allowed them to pinpoint the location and level of stimulation that would activate the central lateral nucleus.
Guided by these models, Henderson surgically implanted the devices in the five participants.
“It’s important to target the area precisely,” he said. “If you’re even a few millimetres off target, you’re outside the effective zone.”
A pioneering moment
After a two-week titration phase to optimise the stimulation, the participants spent 90 days with the device turned on for 12 hours a day.
Their progress was measured by a standard test of mental processing speed, called the trail-making test, which involves drawing lines connecting a jumble of letters and numbers.
“It’s a very sensitive test of exactly the things that we’re looking at: the ability to focus, concentrate and plan, and to do this in a way that is sensitive to time,” Henderson said.
At the end of the 90-day treatment period, the participants had improved their speeds on the test, on average, by 32%, far exceeding the 10% the researchers had aimed for.
“The only surprising thing is it worked the way we predicted it would, which is not always a given,” Henderson said.
For the participants and their families, the improvements were apparent in their daily lives. They resumed activities that had seemed impossible – reading books, watching TV shows, playing video games or finishing a homework assignment. They felt less fatigued and could get through the day without napping.
The therapy was so effective the researchers had trouble completing the last part of their study. They had planned a blinded withdrawal phase, in which half the participants would be randomly selected to have their devices turned off. Two of the patients declined, unwilling to take that chance. Of the three who participated in the withdrawal phase, one was randomized to have their device turned off. After three weeks without stimulation, that participant performed 34% slower on the trail-making test.
The clinical trial is the first to target this region of the brain in patients with moderate to severe traumatic brain injury, and it offers hope for many who have plateaued in their recovery.
“This is a pioneering moment,” Schiff said. “Our goal now is to try to take the systematic steps to make this a therapy. This is enough of a signal for us to make every effort.”
Source: Stanford Medicine

