Until now, the reason why some coronaviruses such as SARS-CoV-2 affect humans more severely than other seasonal ones has eluded scientists. Now, results published in Nature have provided a piece of the puzzle by identifying a gateway used by the seasonal coronavirus HKU1 to enter human cells. HKU1 binds to a different receptor than SARS-CoV-2, which may partly explain the difference in severity between these two coronaviruses.
Receptors provide a useful means of figuring out coronavirus transmissibility and pathology as part of surveillance work on viral evolution. Seven coronaviruses are known for their ability to infect humans. Four of these are generally mild: HKU1, 229E, NL63 and OC43, while the other three are more pathogenic: SARS-CoV-1, Mers-CoV and SARS-CoV-2.
The HKU1 virus was first identified in an elderly patient with severe pneumonia in Hong Kong in 2005. Like SARS-CoV-2, HKU1 mainly infects upper respiratory tract cells. However, it rarely affects the bronchi and alveoli in the lungs. The HKU1 virus causes colds and other mild respiratory symptoms. Complications may also occur, including severe respiratory tract infections, particularly in young children, the elderly and immunocompromised individuals. It is estimated that 70% of children are infected before the age of 6. In total, 75 to 95% of the global population has been exposed to HKU1, which is comparable to other seasonal human coronaviruses.
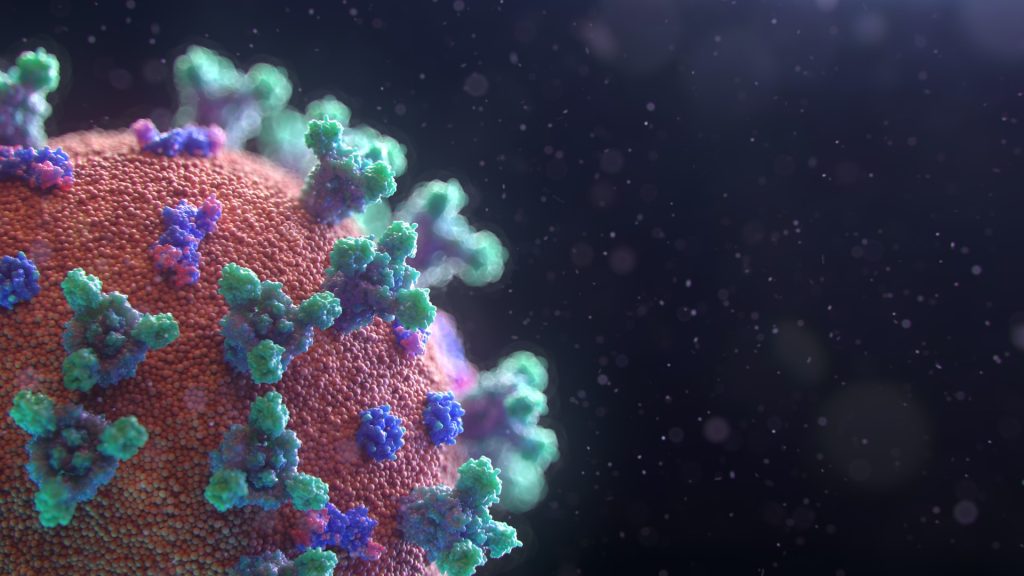
At the cellular level, coronavirus spike proteins are cleaved after binding to their receptors. This cleavage phenomenon is vital for viral fusion, entry and multiplication. Some coronaviruses (SARS-CoV-2 and NL63) use the ACE2 receptor as a gateway for entering cells. Until now, HKU1 and OC43 were the only coronaviruses with unknown receptors.
Through collaboration between scientists at eight Institut Pasteur units, it was possible to identify the TMPRSS2 enzyme as the receptor to which HKU1 binds to enter cells. Once binding has occurred, TMPRSS2 triggers fusion of HKU1 with the cell, leading to viral infection. Through a combination of techniques performed in vitro and in cell culture, the scientists demonstrated that the TMPRSS2 receptor has high affinity with the HKU1 spike, which is not the case for SARS-CoV-2.
“Once a receptor has been identified for a virus, it is possible to characterise target cells more accurately, while also gaining insights on viral entry and multiplication mechanisms and infection pathophysiology,” comments, Olivier Schwartz, co-last author of the study and Head of the Institut Pasteur’s Virus and Immunity unit.
“Our findings also shed light on the various evolution strategies employed by coronaviruses, which use TMPRSS2 either to bind to target cells or trigger fusion and viral entry,” adds Julian Buchrieser, co-last author of the study and scientist in the Institut Pasteur’s Virus and Immunity unit.
These human-pathogenic viruses’ use of different receptors probably affects their degree of severity. Receptor levels vary among respiratory tract cells, thus influencing the sensitivity of cells to infection and viral spread. Once the route of viral entry into cells is known, it should also be possible to fight infection more effectively by developing targeted therapies and assess the risk of virulence posed by any future emerging coronaviruses.
In parallel with this work, Institut Pasteur teams led by Pierre Lafaye and Felix Rey have developed and characterised nano-antibodies (very small antibodies) that inhibit HKU1 infection by binding to the TMPRSS2 receptor. These reagents have been patented for potential therapeutic activities.
Source: Institut Pasteur

