Timed Cortisol Delivery Improves Adrenal Condition Symptoms

A trial of a hormone replacement therapy that more closely replicates the natural circadian and ultradian rhythms of hormones has shown to improve symptoms in patients with adrenal conditions. Results from the University of Bristol-led clinical trial are published in the Journal of Internal Medicine.
Low cortisol levels typically result from conditions such as Addison’s and Congenital Adrenal Hyperplasia. The hormone regulates a range of vital processes, from cognitive processes such as memory formation, metabolism and immune responses, through to blood pressure and blood sugar levels. When low, it can trigger symptoms of debilitating fatigue, nausea, muscle weakness, dangerously low blood pressure and depression. Although rare, these adrenal conditions require lifelong daily hydrocortisone replacement therapy.
Although existing oral hormone replacement treatment can restore cortisol levels, it is still associated with an impaired quality of life for patients. Scientists believe this is because the current treatment does not mimic the body’s normal physiological timing, missing cortisol’s anticipatory rise and lacking its underlying ultradian and circadian rhythms.
The new ‘Pulsatility’ therapy, the culmination of ten years research by the Bristol team, is designed to deliver standard hydrocortisone replacement to patients via a pump which replicates more closely cortisol’s natural rhythmic secretion pattern. The pulsatile subcutaneous pump has now revealed promising results in its first clinical trial.
The double-blinded PULSES six-week trial recruited 20 participants aged 18 to 64 years with adrenal insufficiency conditions. They treated with usual dose hydrocortisone replacement therapy administered either via the pump or the standard three times daily oral treatment.
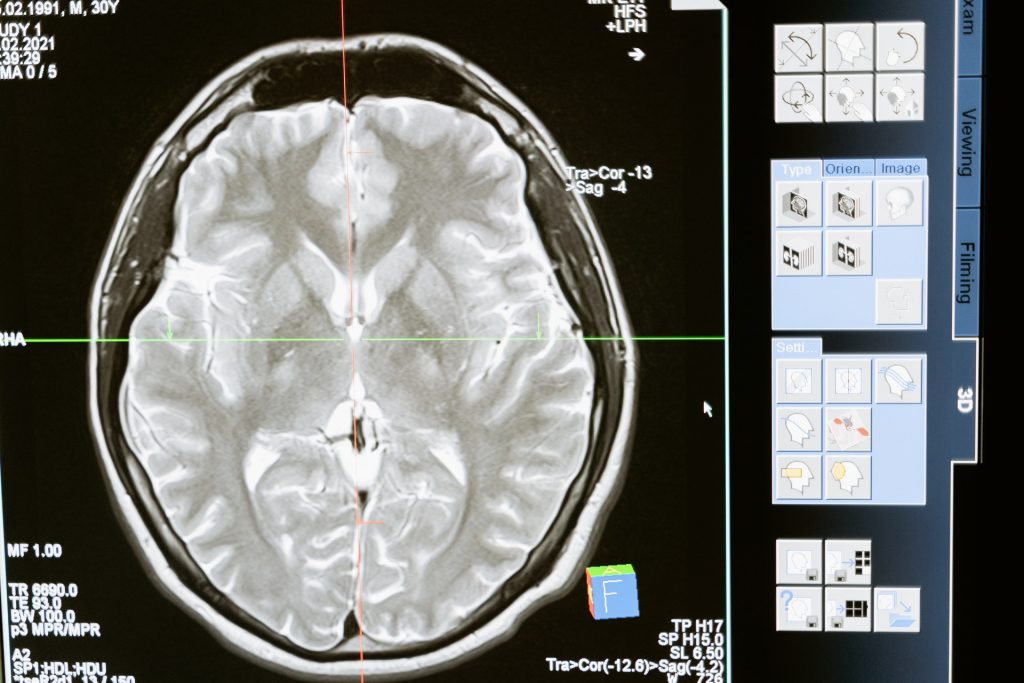
While only psychological and metabolic symptoms were assessed during the trial, results revealed the pump therapy decreased patient fatigue by approximately 10%, improved mood and increased energy levels by 30% first thing in the morning – when many patients struggle the most. MRI scans also revealed alteration in the way that the brain processes emotional information.
Dr Georgina Russell, Honorary Lecturer at the University’s Bristol Medical School, and the lead author, explained: “Patients on cortisol replacement therapy often have side effects which makes it difficult for them to lead normal lives. We hope this new therapy will offer greater hope for the thousands of people living with hormone insufficiency conditions.”
Stafford Lightman, a neuroendocrinology expert and Professor of Medicine at Bristol Medical School: Translational Health Sciences (THS), and the study’s joint lead author, added: “Besides reduction in dosage, cortisol replacement has remained unchanged for many decades. It is widely recognised that current replacement therapy is unphysiological due to its lack of pre-awakening surge, ultradian rhythmicity, and post dose supraphysiological peaks. The new therapy clearly shows that the timing of cortisol delivery, in line with the body’s own rhythmic pattern of cortisol secretion, is important for normal cognition and behaviour.
Source: