Doctors typically treat paediatric ear infections with antibiotics, but children don’t always complete the full course, accelerating resistance to these medications. Today, researchers report developing a single-use nanoscale system that’s unlikely to generate resistance. Using a compound similar to bleach in test animals, they show it can kill off Streptococcus pneumoniae, a common cause of ear infections, and it could someday be easily applied as a gel.
The researchers will present their results at the meeting of the American Chemical Society (ACS).
“We initially conceived of this idea by looking at the household cleaner bleach. Even though it has been used since the 19th century, bacteria do not appear to have developed any widespread resistance to this cleaner,” says Rong Yang, PhD, the project’s principal investigator.
But Yang quickly warns that people should not treat infections with bleach. The solution sold at stores is highly concentrated and caustic, but when used in a properly controlled manner at extremely low concentrations, the active ingredient in bleach is considered compatible with living tissue.
After realising that the active ingredient in the household cleaner could circumvent antibiotic resistance, the Cornell University researchers, set out to tackle a nearly universal childhood scourge: acute ear infections. These infections affect more than 95% of children in the US, and treatment typically requires taking antibiotics for five to 10 days. However, these regimens can cause problematic side effects, leading some families to discontinue the medication prematurely, particularly if symptoms resolve. But using these medications improperly can speed up the development of antibiotic resistance, which makes infections more difficult, if not impossible, to treat. This issue ranks among the biggest threats to global health, according to the World Health Organization.
Bacteria have more success fighting against some substances than others. Hypochloric acid from bleach belongs to a family of compounds, known as hypohalous acids, to which bacteria have yet to develop any significant resistance; most likely because of the numerous ways these highly reactive acids damage microbial cells, Yang says.
Because these substances break down quickly, Yang and her colleagues sought to generate one of them on an as-needed basis behind the eardrum in the middle ear, where ear infections occur. They found inspiration in an enzyme from giant kelp, which converts hydrogen peroxide (H2O2) to hypobromous acid (HOBr), a chemical relative of bleach.
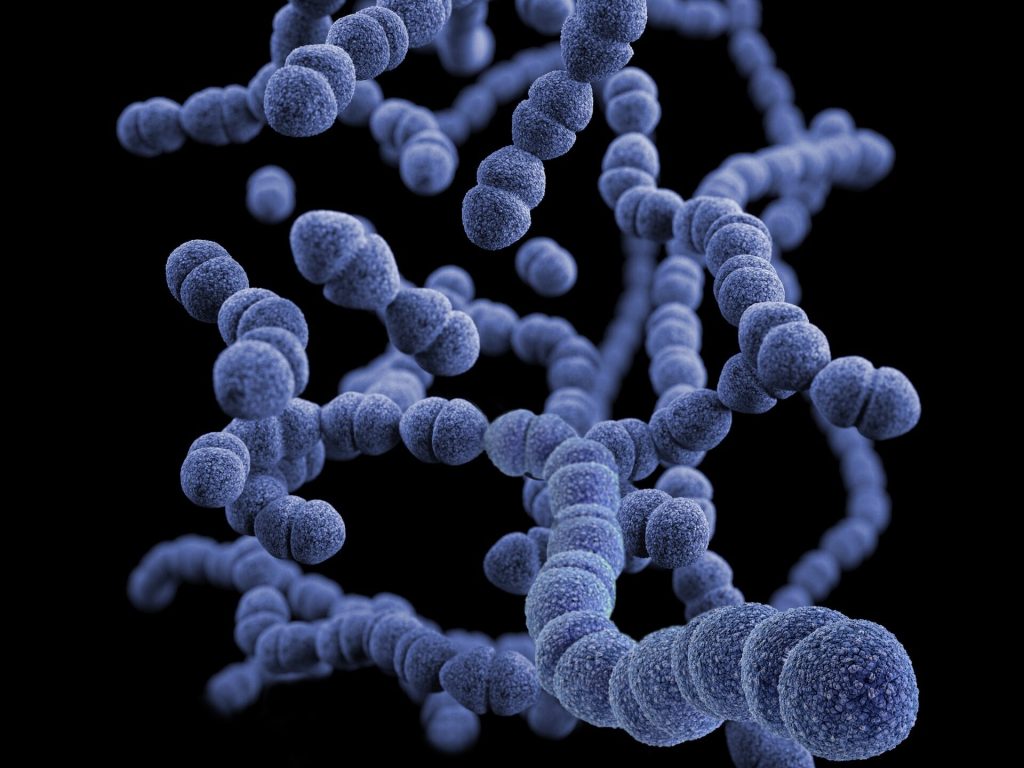
Streptococcus pneumoniae, a frequent cause of ear infections, produces H2O2 to fight off other microbes. To mimic the kelp enzyme, which contains the metal vanadium, Yang and her colleagues designed nanowires made of vanadium pentoxide (V2O5). These produce HOBr only in the presence of the H2O2-producing bacteria, and their rod-like shape helps to keep them in place by reducing their ability to diffuse into body fluids.
In tests on chinchillas, which contract ear infections from the same pathogens as human children, they succeeded in eliminating most of the S. pneumoniae. Yang and colleagues found that after treatment with the nanowires, the animals’ once-inflamed eardrums returned to normal. Meanwhile, tests in healthy animals found evidence that the treatment did not interfere with hearing.
For these experiments, the researchers injected the nanowires directly into the middle ear. In more recent work in chinchillas, they developed a less invasive, more practical method for delivering the wires. By decorating the nanowires with peptides known to transport small particles across the eardrum, Yang and her team found they could deliver the treatment topically as a gel deposited into the ear canal. Once the gel was applied, the nanowires within it went through the intact tissue. They are also exploring other approaches for passing the nanowires through the eardrum.
Because other ear-infection-causing bacteria do not produce H2O2, the researchers are currently examining whether this system is effective in the presence of microbes other than S. pneumoniae, and how they might adapt it to fight the other bugs.
The researchers have not yet done studies to determine how long the system stays in place, although their evidence suggests the nanowires drain out of the middle ear after the infection clears. However, Yang suspects they could adapt the nanowires’ properties to stay in place for long periods afterward. This latter approach could make it possible to prevent recurrent infections that plague many children.
“If the bacteria return, the system could restart, so children wouldn’t need antibiotics repeatedly and breed more resistance along the way,” Yang says.
A video on the research is available at www.acs.org/Earaches.
Source: American Chemical Society

