Cultured Cells may Restore Vision Lost to Photoreceptor Damage
A preclinical study that produced progenitor photoreceptor cells and transplanted them into experimental models of damaged retinas has resulted in significant vision recovery. This finding marks a first step towards potentially restoring vision in eye diseases characterised by photoreceptor loss.
“Our laboratory has developed a novel method that enables the production of photoreceptor progenitor cells resembling those in human embryos,” said Assistant Professor Tay Hwee Goon, first author of the study published in Molecular Therapy. “Transplantation of these cells into experimental models has yielded partial restoration of the retinal function.”
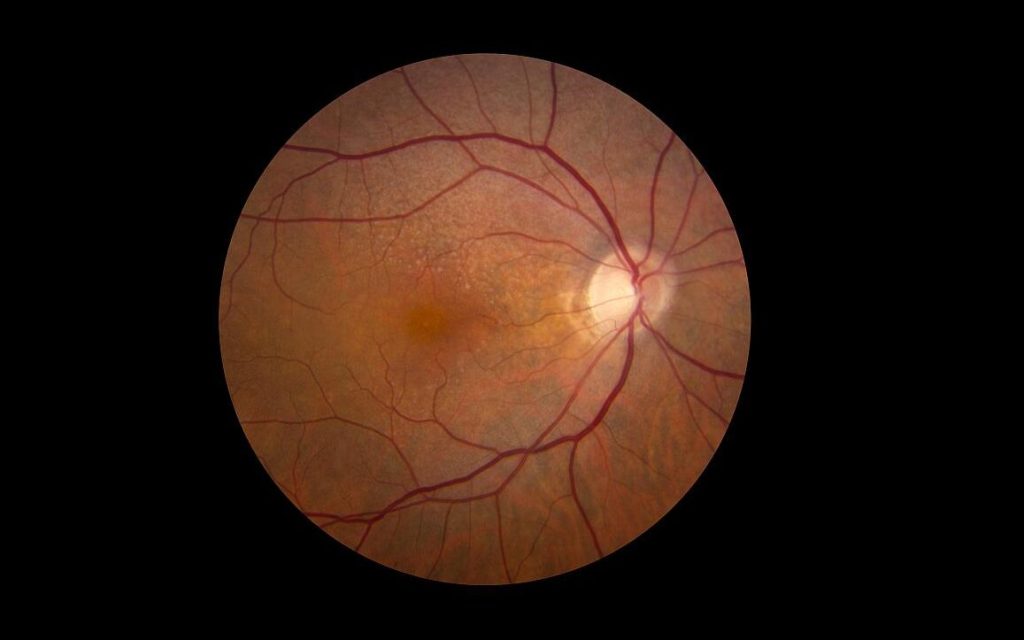
The degeneration of photoreceptors in the eye is a significant cause of declining vision that can eventually lead to blindness and for which there is currently no effective treatment. Photoreceptor degeneration occurs in a variety of inherited retinal diseases, such as retinitis pigmentosa, a rare eye disease that breaks down cells in the retina over time and eventually causes vision loss, and age-related macular degeneration, a leading cause of vision impairment worldwide.
Asst Prof Tay and her team from Duke-NUS Medical School, the Singapore Eye Research Institute and the Karolinska Institute in Sweden, developed a procedure to grow human embryonic stem cells in the presence of purified laminin proteins. These proteins are involved in normal development of human retinas, and in their presence, stem cells could be directed to differentiate into photoreceptor progenitor cells responsible for converting light into signals that are sent to the brain.
When these cells were transplanted into damaged retinas, the preclinical models showed significant recovery of vision. A diagnostic test called electroretinogram also identified significant recovery in the retinas via electrical activity in the retina in response to a light stimulus. The transplanted cells established connections with surrounding retinal cells and nerves in the inner retina. They also survived and functioned for many weeks after transplantation.
Moving forward, the team hopes to refine their method to make it simpler and achieve more consistent results than earlier attempts to explore stem cell therapy for photoreceptor cell replacement.
“It is exciting to find these results, which suggest a promising route towards using stem cells to treat those forms of visual deterioration and blindness caused by the loss of photoreceptors,” said Dr Helder Andre, Head of Molecular and Cellular Research from Karolinska Institute’s Department of Clinical Neuroscience and a senior author of the study.
Associate Professor Enrico Petretto, Director of the Centre for Computational Biology at Duke-NUS and the study’s bioinformatics analysis lead, added: “Our method may also be useful for understanding the molecular and cellular pathways that drive the progression of macular degeneration, perhaps leading to the development of other therapeutic approaches.”
The next challenge for the researchers is to explore the efficacy of their method in models of photoreceptor degeneration that more closely match the human condition.
“If we get promising results in our future studies, we hope to move to clinical trials in patients,” said Professor Karl Tryggvason, from Duke-NUS’ Cardiovascular and Metabolic Disorders Programme, and the corresponding author of the study. “That would be an important step towards for being able to reverse damage of the retina and restore vision.”
Source: Duke-NUS Medical School





