Scientists have shown how tumour cells evade immunotherapy by forming temporary structures, where cells on the inside remain intact and can return to an individual state. These findings, published today in eLife, provide a novel theory as to how tumour cells avoid destruction by the immune system. They could also inform new treatments that combine immunotherapy with the timed inhibition of relevant signalling pathways in tumour cells.
“Cancer immunotherapy harnesses the body’s immune system to fight cancer. Despite its remarkable success, the majority of patients who receive immunotherapy will only see their tumours shrink in size temporarily before returning, and these relapsed tumours will likely be resistant to immunotherapy treatment,” said first author Amit Gutwillig, who was a PhD student at Tel Aviv University when the study was done.
To identify how tumours relapse after immunotherapy, Carmi and colleagues began by comparing the genetic sequences of whole genomes in primary and relapsed tumours in the same patient. Their analysis suggested that relapsed tumours do not change dramatically following immunotherapy.
Next, the team studied this process in breast cancer and melanoma, using mouse models in which immunotherapy-resistant tumours had relapsed. They administered the mice with cells from treated tumours and allowed these cells to reach a palpable size. The team found that the cells were equally susceptible to the same immunotherapy approach as the parent tumour, although they relapsed sooner.
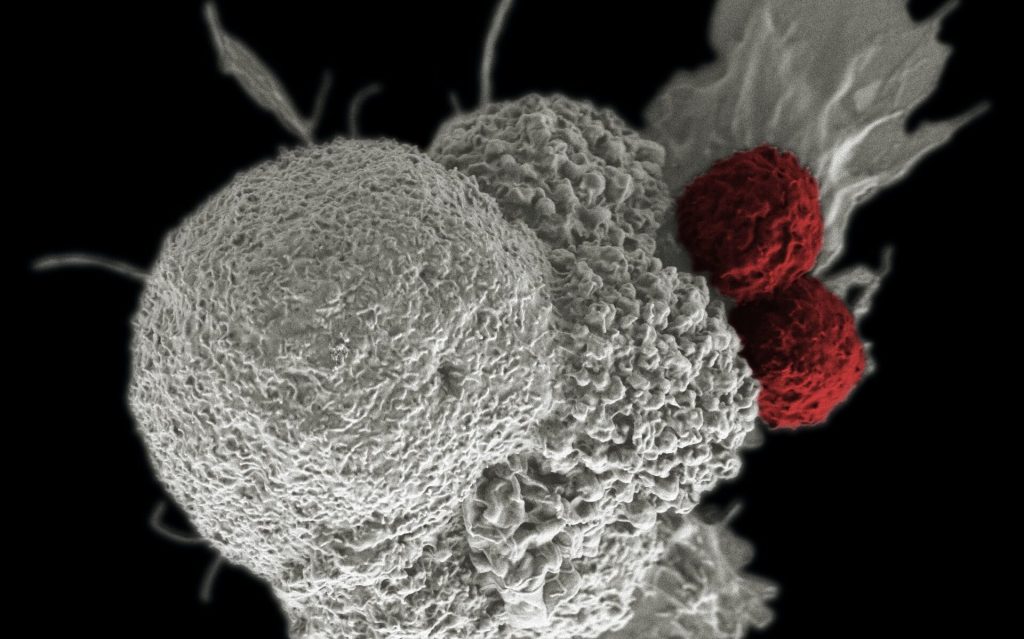
To better characterise the tumour cells that survived in mice following immunotherapy, the researchers isolated and studied the live tumour cells. They found that most of the cells responded to the presence of T cells by organising into temporary formations. These were made up of clusters of several tumour cell nuclei, which are surrounded by a single, multilayered membrane and a meshwork of cortical actin filaments. The inner cell of the formation was dense and appeared to be compacted within another cell.
To show that this result was not due to the isolation of the melanoma cells, the team also analysed tumours with fluorescently labelled cell nuclei and membranes. They found that the cell-in-cell formation was more prevalent in immunotherapy-treated tumours, particularly in sites associated with tumour cell death. Further analysis indicated that roughly half of the tumour cells that survived immunotherapy were arranged in the cell-in-cell formation. Over time, these cells returned to a single-cell state, with similar structural features to those of the parental cell line.
The team next tested whether this phenomenon occurs in human cancers. To do this, they incubated tumour cell lines with pre-activated T cells from healthy donors. They discovered that the vast majority of breast, colon and melanoma tumour cells that survived T cell killing organised into the cell-in-cell structure. A three-day observation of T cells interacting with tumour cells showed that these structures were dynamic, with individual tumour cells constantly forming and disseminating from the structure.
Finally, they tested the clinical relevance of this discovery by analysing cancerous tissues from multiple organs of four stage 4 melanoma patients. These patients were undergoing surgical removal of primary and metastatic lymph nodes. The researchers found that in all four patients, the cell-in-cell formation was highly abundant in the T cell zone of the draining lymph nodes, but not in the primary tumours. Furthermore, in a patient with untreated recurrent melanoma, most of the cells in the primary tumour were single cells, whereas the recurrent tumours had an abundance of the cell-in-cell formations.
“This previously unknown mechanism of tumour resistance highlights a current limitation of immunotherapy,” said senior author Yaron Carmi at Tel Aviv University. “Over the past decade many clinical studies have used immunotherapy followed by chemotherapy. But our findings suggest that timed inhibition of relevant signalling pathways needs to occur alongside immunotherapy to prevent the tumour becoming resistant to subsequent treatments.”
Source: eLife

