Cancer-associated Fibroblasts Sometimes Aid Certain Drugs
Cancer-associated fibroblasts in the tumour environment have typically been linked to tumour progression and therapy resistance, but some studies suggest that these fibroblasts may also sensitise cancer cells to therapy. In a new article published in Science Signaling, researchers shed light on these conflicting studies and demonstrate that cancer associated fibroblasts can promote or inhibit drug sensitivity based on the type of tumour cell and the drug used for treatment.
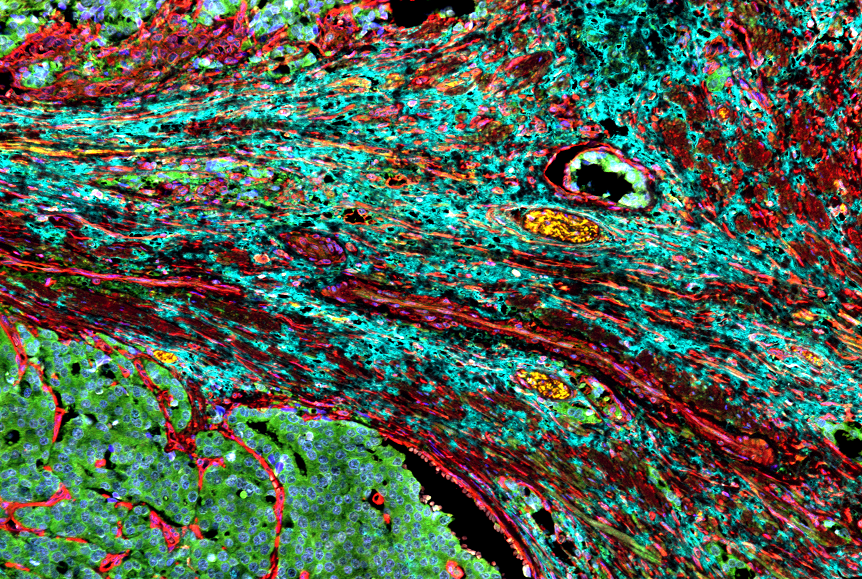
Through a series of laboratory experiments, the research team from Moffitt Cancer Center determined the impact of cancer associated fibroblasts on drug responses among different non-small cell lung cancer (NSCLC) cell lines. They discovered that the presence of cancer-associated fibroblasts had varying effects on tumour cells based on both the type of NSCLC and the drug used for treatment. For example, the presence of cancer associated fibroblasts induced resistance to two different MEK inhibitors in non-small cell lung cancer cell lines with a mutant KRAS protein. However, cancer associated fibroblasts sensitised NSCLC cell lines with a mutant EGFR protein to EGFR inhibitors. Interestingly, normal lung associated fibroblasts never sensitised cells to drug treatment, suggesting that cancer associated fibroblasts secrete a factor that causes differential responses to drug treatment in a cell-context manner.
The researchers compared cancer associated fibroblasts to normal fibroblasts to identify factors that would produce these disparate effects. They found that cancer associated fibroblasts had alterations in the levels of secreted proteins that are part of the insulin-like growth factor (IGF) signalling pathway, which is involved in cell growth, death and migration. Specifically, cancer-associated fibroblasts secreted higher levels of proteins called IGF binding proteins (IGFBPs), which inhibit IGF signalling, and lower levels of IGFs, which activate IGF signalling. In combination, these alterations result in inhibitory effects on the IGF signalling pathway.
In further analyses, the researchers found that IGFBPs sensitised lung cancer cell lines to EGFR inhibitor treatment, while IGF proteins induced resistance to EGFR inhibitor treatment. They identified that survival signalling in response to EGFR inhibitor treatment was dependent on the proteins IGF1R and FAK, which are both part of the IGFBP signalling pathway. Importantly, they discovered that drugs that blocked the activity of IGF1R and FAK sensitised mutant EGFR lung cancer cells to EGFR inhibitors, suggesting that this combination approach may be effective in the clinic.
“These results highlight tumour suppressive effects competing with otherwise tumour promoting effects of cancer associated fibroblasts and add to the growing evidence that eliminating cancer associated fibroblasts in an undifferentiated way may be detrimental to cancer therapy,” said lead study author Lily Remsing Rix, PhD
“We show that mechanistic understanding not just of cancer associated fibroblast-mediated resistance, but also of their tumour suppressive pathways, can lead to rational design of improved therapeutic approaches that mimic these effects and may delay the onset of drug resistance,” added Uwe Rix, PhD, principal investigator of the study.





