The COVID Pandemic has Worsened Antimicrobial Resistance

The COVID pandemic has set back years of progress against antimicrobial resistance, with resistant hospital-onset infections and deaths increasing by at least 15% in the first year of the pandemic alone, according to a new report from the US CDC.
About 3 million people in the US are infected with antimicrobial-resistant pathogens, often acquired in healthcare settings, with about 50 000 people dying. Some estimates predict that by 2050, there could be more deaths from antibiotic resistance than from cancer.
Corrie Detweiler, a professor of molecular, cellular, and developmental biology at CU Boulder, has spent her career trying to develop solutions to antimicrobial-resistance. CU Boulder Today spoke with her about why so many antimicrobial drugs won’t work anymore, how COVID made things worse and what can be done to make things better.
Prior to the pandemic, how were we doing in addressing this issue?
“A lot of progress had been made, particularly in hospital-acquired infections, based on a better understanding of the problem and better guidelines about when to use antibiotics. Between 2012 and 2017, for instance, deaths from antimicrobial resistance fell by 18% overall and nearly 30% in hospitals. That all fell apart during COVID.”
Why? How did COVID spawn an uptick?
We didn’t know how to treat COVID, and, understandably, there was a fair amount of chaos in the medical system. People were using antibiotics more, often inappropriately. About 80% of COVID patients received antibiotics. People were given them prophylactically, prior to knowing they had a lung bacterial infection. That’s not to say that none of (the patients) needed them. Some did. But the more you use antibiotics, the more you select for resistance. And that’s how you eventually get a superbug.
What can society do to address this?
First, we need to go back to this idea of stewardship in hospitals – to only give out antibiotics when there is a clear need. We were doing the right thing. And then something terrible came along and messed it up, and it demonstrated that what we were doing was working well. That’s a good thing. Second, we need to discover and develop novel classes of antibiotics. The last time a new class of antibiotics hit the market was in 1984. The fundamental problem is that they’re not profitable to develop, compared to say a cancer drug. You can go to the drugstore and get a course of amoxicillin for $8. We need programs that reward industry and academic labs like ours for doing the early research.
What does your lab do?
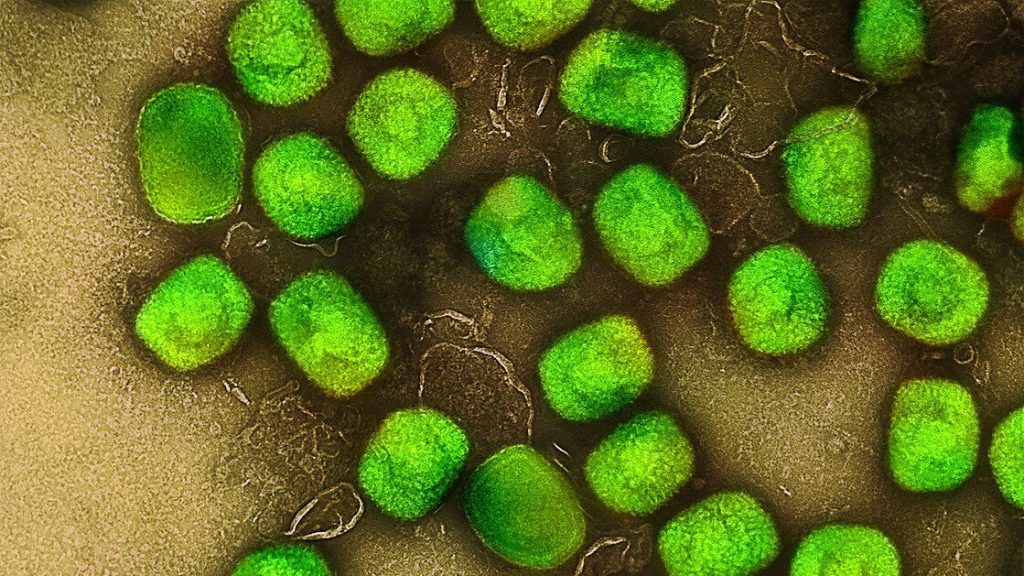
We’re using basic biology to try to figure out new ways to kill bacteria during an infection and identify compounds that work differently than existing drugs.
Source: University of Colorado