Activities That Changed During the Pandemic – and Didn’t Change Back

A new analysis describes how people in the UK shifted the amount of time they spent on various activities over various stages of pandemic restrictions and shifted to online versus in-person settings. The findings were published in the open-access journal PLOS ONE.
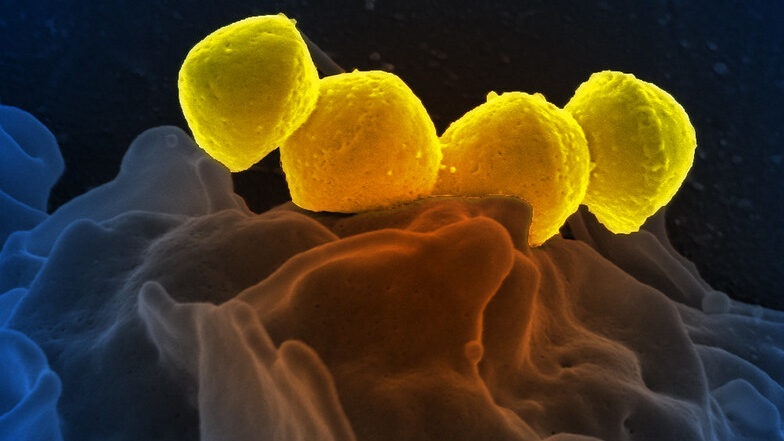
When the COVID pandemic began, the U.K. joined many countries in introducing restrictions on people’s movement and social activities to mitigate viral spread. A growing body of research reveals how such restrictions have affected people’s lifestyles worldwide. This study examined how UK residents’ habits changed over time as different restrictions were implemented and lifted.
The researchers conducted six online surveys of UK residents between April 2020 and July 2021 and were ultimately able to follow 203 people who responded to multiple surveys. The surveys included questions about 16 different types of activities respondents participated in during different phases of the pandemic, such as journalling, shopping, and getting active, and whether they participated online or in person.
Statistical analysis of the responses showed that the biggest changes in terms of amount of time spent – as well as the biggest changes in online versus in-person participation – occurred for cultural activities, spending time with others, and travelling. Changes were most pronounced in March to June 2020, corresponding with the first lockdown period, when participation in all 16 activities decreased. The biggest shift from in-person to online participation occurred from March to October 2020, which included the first lockdown followed by relaxation of restrictions.
Cultural activities, such as going to museums, and group activities were the two categories that fell the most, and did not recover to pre-pandemic levels when UK restrictions were lifted on July 19, 2021. During the restrictions, participation was mostly online in these activities. Spending time with family was among the most robust, and remained mostly in-person, though supplemented by online interaction.
These findings could help policymakers understand the impact of their pandemic restrictions. In the future, the researchers plan to investigate how demographic factors, such as age and employment, may have affected the results, as well as long-term mental health implications of the lifestyle changes.
Professor Patty Kostova, leader of the study, added: “This longitudinal research study illustrated citizens’ resilience throughout the stages of the pandemic.”
Lan Li adds: “This longitudinal study determines the frequency and way of people doing activities from Spring 2020 to Summer 2021 during different phases of the COVID pandemic in the UK. The findings provide an invaluable insight into understanding how people in the UK changed their lifestyle, including what activities they do, and how they accessed those activities in light of the COVID pandemic and related public health policy implemented to address the pandemic.”
Source: ScienceDaily