Mutations that Predispose Patients to Severe Staph Infection
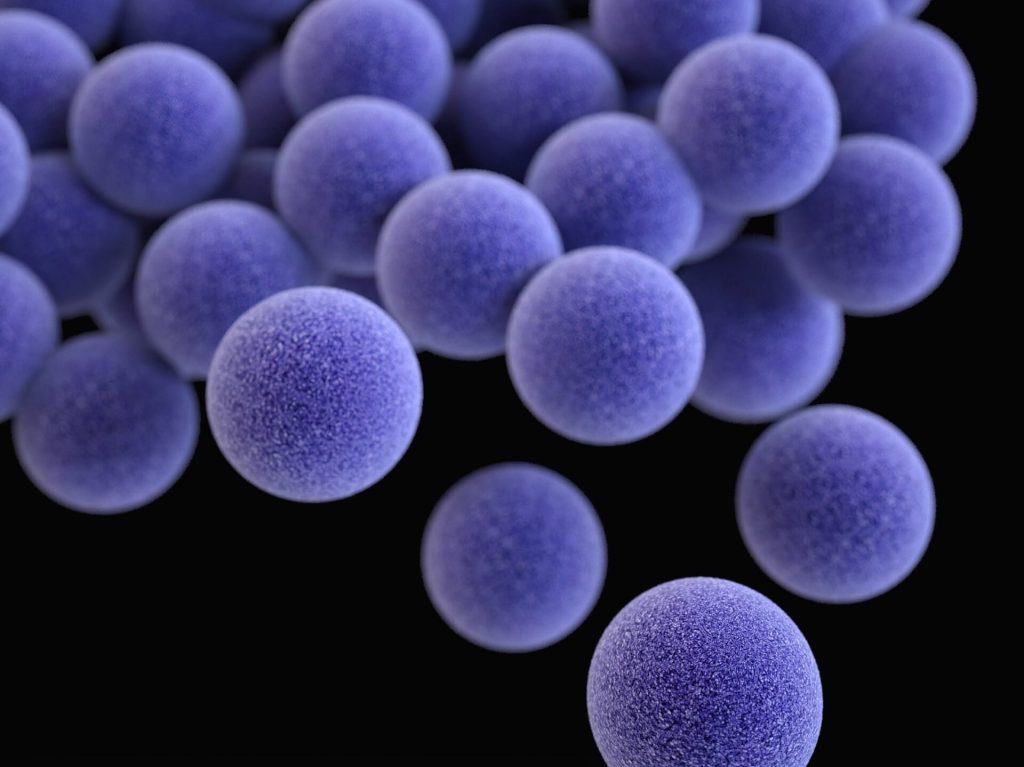
A common culprit of skin and respiratory infections, Staphylococcus aureus is highly unpredictable, with the bacteria mostly harmlessly present in the skin of 20–30% of people. However, these bacteria can occasionally cause infections that lead to deadly complications, such as pneumonia, deep skin infections, and sepsis. This was a totally unpredictable outcome – until now.
Now, a new study published in Science identifies a mutated gene common to multiple patients who suffer life-threatening infections and suggests that people living with a genetic condition known as 5p- or Cri-du-chat syndrome may be at similar risk.
“We have characterised severe Staphylococcus aureus infection at the genetic, cellular, immunological, and clinical levels,” said András Spaan, the study’s first author. “By integrating these levels, we have established causality and provided clues for future interventions.”
A first for cell intrinsic immunity
To find out why S. aureus causes disease in some people but not others, scientists examined the protein-coding genomes of more than 100 patients who had suffered from unexplained severe staph infections.
The common genetic thread linking some of these disparate patients were mutations of a gene called OTULIN, which is perched along the short arm of chromosome 5 and codes for an enzyme involved in regulating inflammation. These individuals were not entirely bereft of OTULIN –only one of their two copies of the gene was mutated – but that deficiency appeared to be all it took to render them vulnerable to infections that would scarcely harm other people.
The scientists expected to find that OTULIN deficiency somehow cripples white blood cells or otherwise prevents the immune system from snuffing out S. aureus. But further investigation revealed that these mutations indirectly cause an unrelated protein to aggregate on the surfaces of skin and lung cells, gumming up the tools that those cells use to defend themselves from a toxin produced by S. aureus. This mechanism of defense is known as cell intrinsic immunity.
This finding was particularly surprising because, until then, specific defects in cell intrinsic immunity had only been linked to a predisposition to some viral infections, from COVID to herpes to encephalitis. It had never been shown to play a role in bacterial disease. “This is the first known instance of cell intrinsic immunodeficiency predisposing patients to bacterial infection,” Spaan says.
A larger role for OTULIN
While the individuals whom Spaan and colleagues studied were only missing one copy of OTULIN, people born without either functional copy of this gene face a bevy of early-onset inflammatory diseases, which often prove fatal in the first year of life.
This observation led Spaan to conclude that one functional copy of OTULIN is enough to prevent inflammatory disease, but insufficient to protect against life-threatening staph infections—a genetic mechanism known as haploinsufficiency. “The genetic mechanism was important to pin down,” Spaan says. “People with two functional copies of the gene appear to be healthy, those with no functional copies have autoinflammatory disease, and those with one functional copy are susceptible to severe staph infections.”
Given that general rule, the researchers hypothesized that any population missing only one copy of OTULIN would be similarly predisposed to severe infections. So they then examined a group of volunteers with 5p- syndrome, the most common chromosomal deletion disorder in humans characterized by developmental delays, intellectual disabilities and, in infants, a high-pitched cry. Most 5p- syndrome patients are missing the entire short arm of chromosome 5 and therefore invariably go about their lives with only one functional copy of OTULIN.
Indeed, upon examining six 5p- syndrome patients, the team found that one third were susceptible to lung infections. “We were able to demonstrate that this susceptibility is driven by the fact that they had only one functional copy of OTULIN,” Spaan says. “In many ways, these patients looked genetically similar to the patients we had identified with severe staph infections.”
“Both clinically, and on the cellular level, they could almost be said to have the same disease.”
The findings do not imply that everyone with OTULIN haploinsufficiency or 5p- syndrome will contract severe infections. In fact, the initial results of the study suggested that only 30 percent of individuals with these mutations develop severe disease. Why OTULIN haploinsufficiency appears to cause disease in some patients but not others—a common phenomenon that genetics researchers call “incomplete penetrance”—will be the subject of follow-up studies.
“Many genetic disorders act in this way, but it remains puzzling,” Spaan says. “Why are some people with these mutations perfectly healthy, while others get super ill and may even die?”
One potential answer has already surfaced. Spaan and colleagues found that individuals with OTULIN mutations but no sign of severe disease had high levels of antibodies that neutralise the toxin produced by S. aureus, perhaps due to prior exposure to the common skin bacteria. Individuals with severe disease, on the other hand, had precious few antibodies.
Further investigation into genetic predisposition to diseases, particularly ones as stubborn as staphylococcal infections, may help the development of future treatments. “Studies on these disorders can act as a compass,” Spaan said, “Our research clarifies the interactions between hosts and pathogens, revealing scientific insights into pathogenesis and immunity.”
Source: Rockefeller Institute





