Researchers Identify a Key Regulatory Mechanism in Inflammation

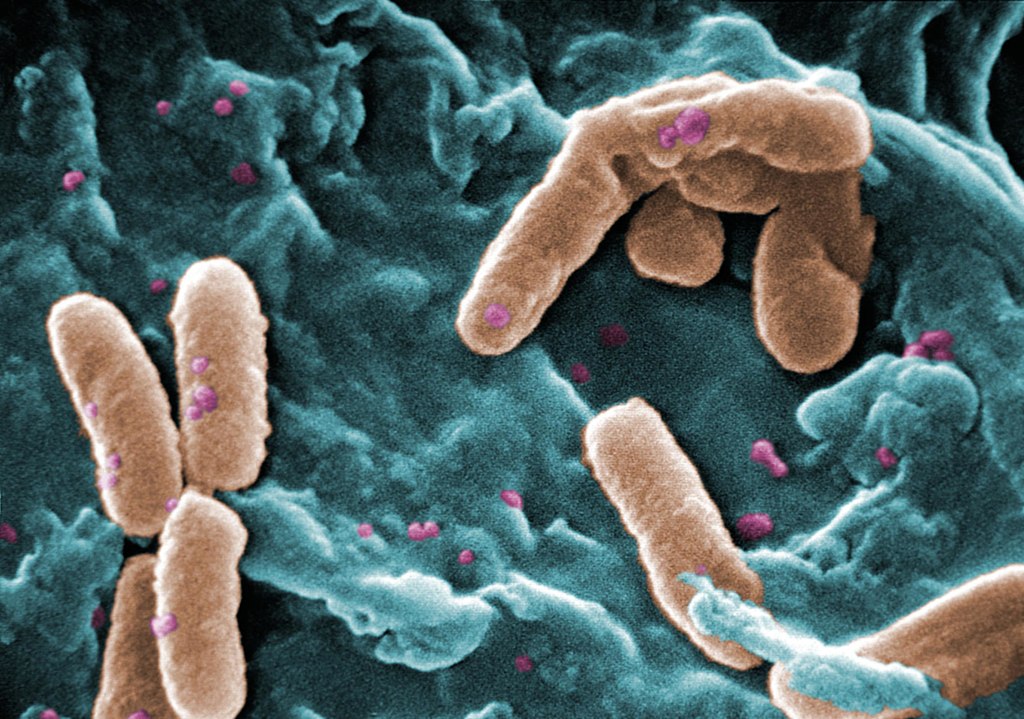
A newly published study has identified a key regulatory mechanism in inflammation that may lead to new targets for resolving that inflammation –and the inflammation of patients with sepsis, cancer and COVID.
In the journal PNAS, scientists reported their discovery of a regulatory pathway for immune response after infection or injury, such as burns. Dysregulation of this pathway could differentiate those who are at risk of fatal sepsis or help identify targets to resolve this unregulated inflammation.
“We are very excited about the findings in this paper and the far-reaching impacts it could have on understanding a key regulatory step in the immune response,” said co-lead author Cindy McReynolds, who holds a doctorate in pharmacology and toxicology.
In a rodent model, the research team found that the metabolites of linoleic acid formed by the enzyme, soluble epoxide hydrolase (sEH), drive damaging inflammation after injury. These metabolites, known as lipid mediators, regulate inflammation, blood pressure and pain. Drugs that inhibit the sEH enzyme and reduce inflammation could lead to better outcomes.
“Our previous work identified that these same lipid mediators were up-regulated in severe COVID infections, and we are now finding that these compounds play a role in modulating the immune response so that the body is unable to fight infection or respond properly to trauma without leading to a potentially fatal overreaction,” said Dr McReynolds.
“This dysregulation has fatal consequences in serious diseases such as COVID, cancer, sepsis, burn, where fatality rates can be as high as 40 percent in severe cases,” she said. “An understanding of these pathways can help identify patients at risk of developing serious disease or identify new therapeutic targets for treatment.”
“The immunological disbalance we see in many cases of severe burn injury, trauma and sepsis pose a huge clinical challenge as we lack the understanding of how to diagnose and treat it,” explained co-lead author Dr Christian Bergmann. “With this work, we reveal an important mechanism how immune cells are functionally disabled by sEH-derived metabolites of linoleic acid.”
“The natural compounds we are studying in this paper are metabolites of linoleic acid (LA), an essential fatty acid the body needs in very small amounts to survive and is only available through the diet,” Dr McReynolds elaborated. “At lower concentrations, these metabolites are necessary for regulating thermogenesis and heart health but promote inflammation at higher concentrations. LA is more stable and much cheaper than longer chain polyunsaturated fatty acids, so heavily processed foods have higher LA content to increase shelf-life. Additionally, agricultural practices, such as feeding animals corn-based diets, have increased LA in meats and dairy products.”
“As a result, we are consuming the highest amount of linoleic acid and have the highest recorded concentration of LA in our fatty tissue in human history,” McReynolds said. “As our bodies respond to stress or disease, we metabolise LA into the regulatory metabolites that were monitored in this paper. At higher concentrations, the immune system was unable to properly respond to infection, thereby promoting a sustained immune response. These observations are important in inflammatory-driven diseases, such as sepsis and COVID, but could also be important in understanding many of the increased chronic diseases we are seeing in our population.”
Source: UC Davis