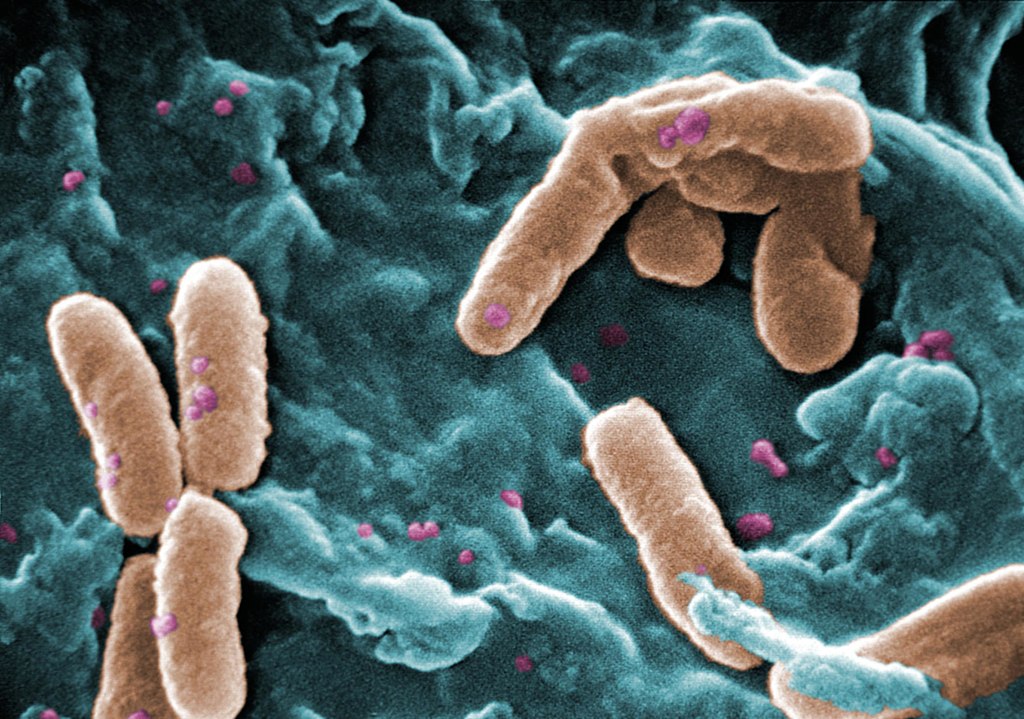
Credit: CDC/Janice Carr
While pathogens usually work against drug treatments, sometimes, they can actually strengthen them, according to a new University of Maine study published in the journal Infection and Immunity.
Polymicrobial infections, which are a combination of bacteria, viruses, fungi and parasites, are challenging to treat because it is not well understood how pathogens interact during infection and how these interactions affect the drugs treating them.
In a study published in Infection and Immunity, University of Maine researchers examined two common pathogens that often occur at similar sites, particularly in cystic fibrosis and mechanically ventilated patients: Candida albicans and Pseudomonas aeruginosa.
Candida is the fourth most common hospital-acquired pathogen, and many antifungal agents only slow it rather than kill it outright. Meanwhile, P. aeruginosa infects 90% of all adult cystic fibrosis patients. Combined, C. albicans and P. aeruginosa cause more serious disease in cystic fibrosis and ventilated patients.
The researchers investigated the effectiveness of the antifungal drug fluconazole in vitro and then during infection of the zebrafish with both pathogens. Fluconazole slows fungal growth, but Candida can become tolerant to the drug and not only survive, but also evolve tolerance that leads to therapy failure and, potentially, death.
The results showed that P. aeruginosa in fact works with fluconazole to eliminate drug tolerance and clear the C. albicans infection in the culture and the zebrafish.
“Polymicrobial infections are challenging to treat not only because of the lack of understanding of how invading microorganisms interact but also because we don’t know how these interactions affect treatment efficacy. Our work demonstrates that polymicrobial interactions can indeed affect treatment efficacy and, most importantly, it highlights the importance of nutrient availability in the environment -; such as iron in our study -; and how it modulates treatment efficacy,” explained Siham Hattab, lead author of the study.
What’s more, the bacteria also enhance the drug’s ability against a second pathogenic Candida species that tends to be more resistant to the drug.
The increased effectiveness of the drug suggests to the researchers that there is still much more to learn about how current drugs work when targeting these dangerous and complex polymicrobial infections.
Senior study author, Robert Wheeler, associate professor of microbiology said: “We are really excited to have revealed that sometimes drugs against fungal infection can work even better in a more ‘real-world’ situation than in the test tube. There is still a lot to learn about how pathogens interact during infection, and it will be interesting to see how the bacteria manage to work with the drugs to target Candida.”
Source: University of Maine

