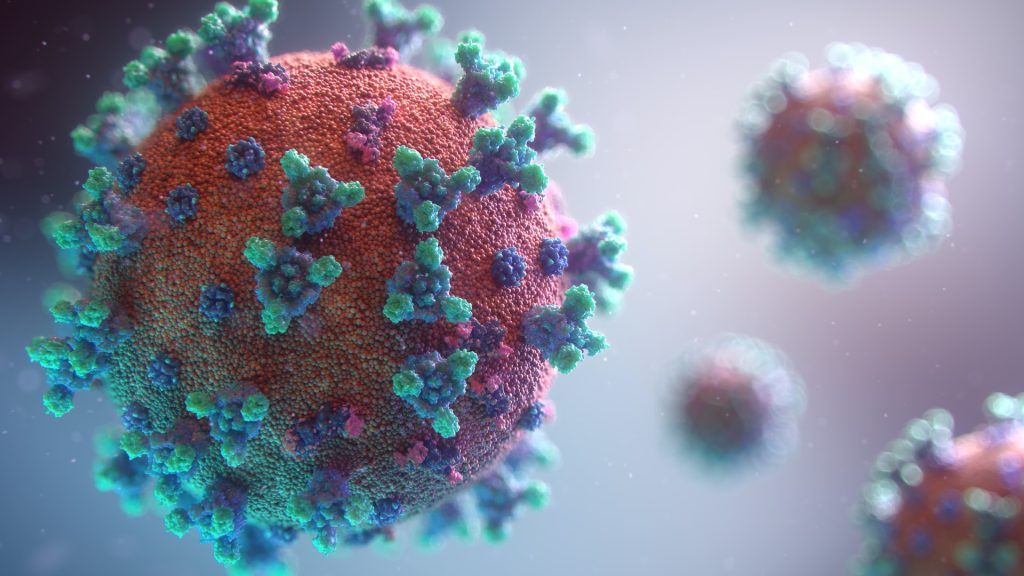
Using in vitro modelling the SARS-CoV-2 infection of human pancreatic cells, researchers have found that COVID infection is likely not associated with an increased new-onset diabetes risk. At the same time, another study has suggested that in hospitalised COVID patients, it may be a temporary form of the disease resulting from the acute stress of viral infection.
The findings, which are to appear in Cell Reports, address concerns raised over the past 18 months that infection with SARS-CoV-2 may trigger new-onset diabetes. However, the supporting evidence for this has remained sparse, with at times conflicting evidence impeding with a proper risk assessment.
The team of researchers at the Icahn School of Medicine at Mount Sinai demonstrated that SARS-CoV-2 targets virtually all types of pancreatic cells, not just the insulin-producing beta cells, using the ACE2 receptor to gain access. However, the infection in the pancreas remained highly circumscribed, largely non-cytopathic and despite high viral burden in infected subsets, promoted only modest cellular perturbations and inflammatory responses.
Similar experimental outcomes were also observed after in vitro infection with endemic coronaviruses not previously associated with diabetes. Taken together, these findings challenge the notion that direct beta cell infection and destruction by SARS-CoV-2 can precipitate diabetes onset.
“Our provisional conclusions indicate that SARS-CoV-2 infection is likely not associated with an increased risk for new-onset diabetes,” said study leader Dirk Homann, MD, Professor of Medicine at Icahn Mount Sinai. “However, a history of SARS-CoV-2 infection may yet promote prolonged glycometabolic perturbations and even an increase in cumulative diabetes risk in vulnerable populations. Over the next few years, we need to pay careful attention to emerging observational and retrospective studies that determine diabetes incidence rates of previously SARS-CoV-2-infected individuals.”
To evaluate permissiveness of human pancreatic islet cells to in vitro SARS-CoV-2 infection, the team of researchers employed an in vitro infection model of primary human pancreatic islets with SARS-CoV-2 as well as endemic human coronaviruses. The team precisely delineated pancreatic infection patterns and associated cellular changes at the single-cell level. Altogether, they found that the extent and consequences of pancreatic SARS-CoV-2 infection, even under in vitro conditions of enhanced virus exposure, remained decidedly limited.
“Concerns surrounding the possibility that infection with SARS-CoV-2, the etiological agent of COVID, may cause new-onset diabetes persist amidst an evolving research landscape,” said Verena van der Heide, MD, PhD, co-first author of the study and postdoctoral research fellow at the Icahn School of Medicine at Mount Sinai. “Our findings stand in notable contrast to three recent reports that also based their speculation about the diabetogenic potential of SARS-CoV-2 on in vitro infection of human islets. As detailed in our manuscript, however, we believe that our careful experimental design and comprehensive analysis strategy make a compelling case for the considerable limits of pancreatic SARS-CoV-2 infection.”
“There are strong epidemiological associations between COVID infection in humans and diabetes, but whether the SARS-CoV-2 virus actually infects and damages the insulin-producing cells in the human pancreas, the so-called ‘beta cells,’ has been highly controversial,” said Andrew Stewart, MD, Director of the Diabetes, Obesity and Metabolism Institute at Icahn Mount Sinai. “This study by Dr. Homann and his collaborators in Mount Sinai’s Precision Immunology Institute and the Department of Microbiology provides strong evidence that SARS-CoV-2 causes little or no damage to beta cells, making it unlikely that COVID infection can predispose to development of Type 1 diabetes.”
The conclusions they came to are in line with a 2020 report by Dr Homann and his team, showing that ACE2 receptors and other entry factors are lacking among islet endocrine cells but readily detected in microvascular and ductal structures of the pancreas.
Meanwhile, a second, separate study of 594 individuals who exhibited signs of diabetes mellitus during the early pandemic showed that half of the 79 patients without a diabetes diagnosis reverted to normal blood sugar levels by one year.
“We believe that the inflammatory stress caused by COVID may be a leading contributor to ‘new-onset’ or newly diagnosed diabetes,” said Sara Cromer, MD, lead author of the second study. “Instead of directly causing diabetes, COVID may push patients with pre-existing but undiagnosed diabetes to see a physician for the first time, where their blood sugar disorder can be clinically diagnosed. Our study showed these individuals had higher inflammatory markers and more frequently required admission to hospital ICUs than COVID patients with pre-existing diabetes.”
The second study was published in the Journal of Diabetes and its Complications.
Source: Mount Sinai Medical Center


One Reply to “COVID Infection not Associated With Increased New-onset Diabetes Risk”
Comments are closed.