In Severe Stroke, Mechanical Clot Removal Leads to Improved Outcomes

Copyright American Heart Association
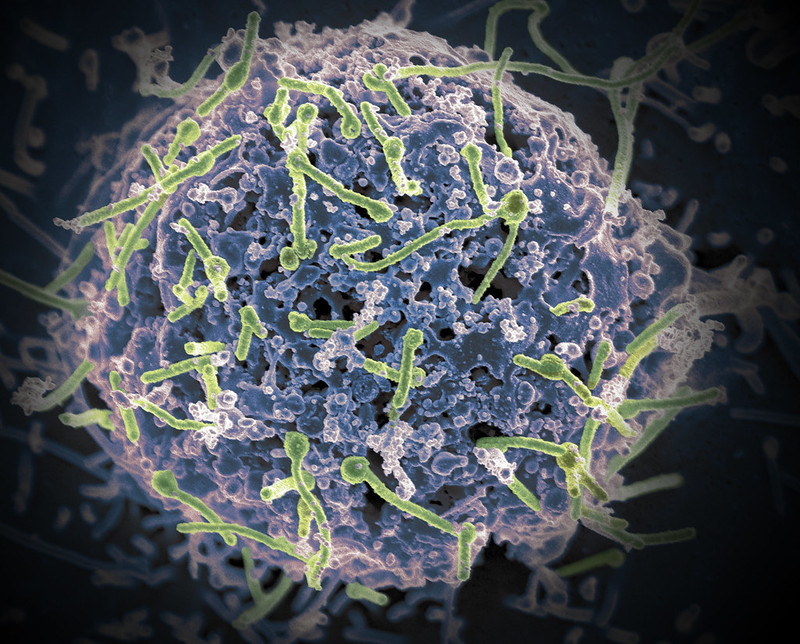
Ischaemic stroke patients previously considered unlikely to survive without severe disability may regain far more function if the blood clots are mechanically removed in addition to standard medical therapy, according to preliminary late-breaking research presented today at the American Stroke Association’s International Stroke Conference 2022.
In 2018, the American Heart Association’s stroke treatment guidelines were updated to recommend endovascular therapy (mechanical clot removal) for select stroke patients to improve the odds of functional recovery. This new study in Japan is the first randomised, controlled trial to demonstrate the effectiveness of endovascular therapy in patients with severe strokes involving clots in one or more large brain arteries, causing a large blood flow interruption in the brain. This approach had worked for patients with fewer areas of the brain disrupted, however, clinical experience was mixed for patients with more severe strokes.
Infarction area, or core area, estimates the volume of brain affected and describes the blockage location as seen on a brain CT. A lower number translates to a stroke affecting more core areas of the brain: 8-10=small core, 6-7=moderate core and 0-5=large core. Current US stroke guidelines recommend endovascular therapy for core areas 6-9. This study examined blockages that scored as 3-5. Strokes with blockages measuring 0-2 core areas are considered too severe and highly unlikely the patient would return to ambulatory independence.
“I have often encountered a dramatic improvement in a patient just after the mechanical clot removal procedure, even when the infarction area was large. Yet, patients sometimes also experienced severe haemorrhagic transformation [a life-threatening complication that occurs when blood from outside the brain crosses the blood-brain barrier and worsens stroke outcome] after the artery was reopened. So, in Japan, our stroke physicians are always cautious about endovascular therapy when the infarction area is large,” said Professor Shinichi Yoshimura, lead author of the study.
This randomised study included 203 stroke patients (average age of 76 years; 44% women). Most (71%) were examined and had MRI or a CT scan of the brain within 6 hours after stroke symptoms were first noticed, when patients are generally considered eligible for endovascular therapy. The other patients were seen between 6-24 hours after symptoms were noticed, and additional imaging showed areas of the brain that might benefit from prompt treatment.
On imaging, all patients were found to have clots blocking a large cerebral artery – either the internal carotid artery, the proximal middle cerebral artery or both. The strokes were rated as severe (median 22 on the National Institutes of Health (NIH) Stroke Scale,) and involved disrupted blood flow to large areas of the brain (about 7 out of 10 regions).
After imaging, the patients were randomly selected to receive either standard medical care for stroke (intravenous fluids, controlling blood pressure and other risk factors, and thrombolytics for lower bleeding risk patients) or standard medical care plus endovascular therapy performed within an hour after imaging to mechanically remove the clots. Due to bleeding concerns, intravenous thrombolytics were sparingly administered to select patients in a similar proportion in both treatment groups (27 of those who received endovascular therapy and 29 who received standard care).
Comparing the 100 patients who received endovascular therapy with 102 on standard therapy alone, the analysis found:
- Patients who received endovascular therapy were 2.43 times more likely (31% vs 13%) to be able to walk unassisted and to have a residual disability rated as none to moderate 90 days later.
- After 90 days, more of the patients (14% vs. 6.9%) who received endovascular therapy were considered functionally independent, meaning they were either able to carry out all their pre-stroke activities or to have a slight disability that did not require daily assistance.
- At 48 hours after treatment, more of the patients (31% vs. 8.8%) who received endovascular therapy had major early neurological improvement.
“Our findings confirm that anyone who suffers from stroke should be transferred to a medical facility capable of endovascular therapy as soon as possible. The benefit of endovascular therapy is not limited by the severity or region of a stroke. These patients may have the chance to more fully recover from stroke and go back to their previous lives and activity levels,” said Professor Takeshi Morimoto, senior author of the study.
Several outcomes were compared to evaluate the safety of adding endovascular therapy to medical treatment, with researchers reporting:
- Within 48 hours, scans revealed that more of the patients who received endovascular therapy had experienced some bleeding within the brain (with or without symptoms), 58% vs. 31%, respectively.
- However, the number of patients who experienced other adverse outcomes was similar in the two treatment groups. The adverse events included brain bleeding within 48 hours that caused a worsening of neurological status (4 points or greater worsening on the NIH Stroke Scale); the need for surgery to relieve pressure on the brain in the first week; death within 90 days; or the recurrence of ischaemic stroke within 90 days.
“The finding of more intracranial bleeding in the patients who received endovascular therapy is very important. However, there were haemorrhages with symptoms and some that caused no symptoms. The haemorrhages with no symptoms were detected on imaging conducted for this study in the endovascular treatment group, not in the standard practice group. Symptomatic intracranial haemorrhage still occurred more commonly among patients in the endovascular group, however, it was not a statistically significant difference from the standard care group,” Morimoto said.
Due to different treatment protocols in Japan, where there is less use of intravenous thrombolysis than in the US and other western countries, and where more strokes are imaged with MRI than CT, this study’s results may over- or underestimate the effectiveness of endovascular therapy.
The researchers are currently performing sub-analyses to help identify factors that might signal which patients are more likely to have a greater return of function after the treatment. “In addition, tools, devices or rehabilitation methods that could potentially improve the likelihood for similar patients to recover with less disability should be investigated,” Morimoto said.
Source: American Heart Association