MMR and Tdap Vaccines May Confer Some COVID Protection

Mounting evidence shows that the Measles-Mumps-Rubella (MMR) and Tetanus-Diphtheria-Pertussis (Tdap) vaccines confer limited protection against COVID.
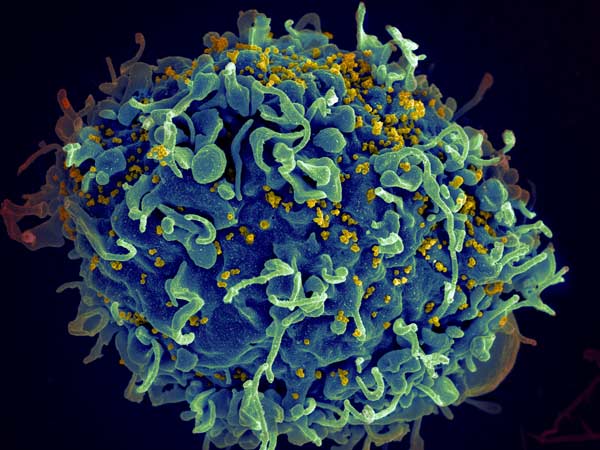
The MMR vaccine, given during early childhood, and Tdap vaccine, given every 10 years, elicit protective responses against the diseases they are designed for. It’s possible that they also elicit cross-reactive memory T cells that can respond to antigens that are present in other pathogens — including the viral antigens in SARS-CoV-2. The idea is that pre-existing memory T cells generated by prior MMR or Tdap vaccination and activated by SARS-CoV-2 infection give the immune system a head start in responding to SARS-CoV-2, lowering the risk of severe COVID.
To find out if the MMR and Tdap vaccines provide additional protection against COVID, researchers at Brigham and Women’s Hospital performed laboratory-based analyses with new techniques to detect and characterise T cell responses to antigens. They applied these techniques to measure T cell responses isolated from the blood of COVID convalescent patients and patients vaccinated against COVID to antigens from SARS-CoV-2 and the MMR and Tdap vaccines. They also leveraged a large, well-annotated cohort of COVID patients and found that prior MMR or Tdap vaccination was associated with decreased disease severity. Their results are published in Med.
“Our Cleveland Clinic colleagues observed an association where individuals with COVID who had either MMR or Tdap vaccines had a much lower frequency of going to the intensive care unit or dying,” said co-author Andrew Lichtman, MD, PhD, an immunologist and senior investigator in the Brigham’s Department of Pathology and professor of Pathology at Harvard Medical School. “Although previous smaller studies suggested a similar link, our in-depth epidemiological analyses, together with our basic research results, suggest that these commonly given vaccines may protect against severe disease.”
“During the COVID pandemic, we know that there was a marked decline in routine vaccinations for children and adolescents,” said corresponding author Tanya Mayadas, PhD, a senior scientist in the Brigham’s Department of Pathology and professor of Pathology at Harvard Medical School. “Our findings emphasise the importance of routine vaccination for children and adults. We know vaccines protect against devastating diseases, and we’re now seeing growing evidence that some of them provide a degree of protection against severe COVID disease.”
An unexpected observation jumpstarted the investigation. Prof Mayadas, her postdoctoral fellow Vijaya Mysore, PhD, and colleagues noted in lab experiments with COVID convalescent blood that whenever they observed a heightened T cell response to SARS-CoV-2 proteins, they also saw a heightened response to proteins from MMR and Tdap, which were controls. This was seen in both COVID convalescent and uninfected individuals vaccinated against SARS-CoV-2.
In a subsequent analysis, Prof Mayadas and colleagues teamed up with researchers at Cleveland Clinic to examine the epidemiological evidence. The Cleveland Clinic team performed a retrospective cohort study using data from more than 75 000 patients seen at the Cleveland Clinic Health System in Ohio or Florida who had tested positive for COVID between March 8, 2020, and March 31, 2021. A statistical analysis found that patients who had previously been vaccinated for MMR had a 38 percent decrease in hospitalisation and a 32 percent decrease in ICU admission/death. Patients previously vaccinated for Tdap had 23 percent and 20 percent decreased rates, for these outcomes, respectively.
“Beyond learning about the potential benefits of the MMR and Tdap vaccines in the context of COVID, this study provides a blueprint for accelerating research,” said co-author Lara Jehi, MD, MHCDS, Chief Research Information Officer of the Cleveland Clinic Health System. “Biomedical hypotheses generated in the laboratory can be explored through robust clinical and epidemiological research in well-curated, real-world data such as the Cleveland Clinic COVID Registry. Knowledge learned through this collaboration is much more than the sum of our individual parts.”
The authors note that epidemiological observations strengthen their lab findings, more work is needed to find a causal association between the MMR and Tdap vaccinations and severity of COVID disease.
“With regards to COVID vaccines, our findings predict that although MMR and Tdap are not a substitute for COVID vaccines they may afford greater and more durable protection, possibly against emerging spike variants than the COVID vaccine alone,” said Prof Mayadas. “And in areas where the COVID vaccines are not available, they could protect infected individuals from developing severe disease.”
Source: Brigham and Women’s Hospital