C.1.2 Variant Slows in SA; Colombian Variant Named Mu

The Network for Genomic Surveillance in South Africa (NGS-SA) has reported that the C.1.2 variant is spreading less slowly than in July, from 2.2% of all sequenced COVID cases to 1.5% in August, and is therefore unlikely to become a dominant variant.
Meanwhile, B.1.621, another variant that first emerged in Colombia in January has been recently classified by the World Health Organization (WHO) as a variant of interest (VOI), receiving the Greek letter “Mu”. Since its first detection, it has spread across North America, South America and Europe, and has also been detected in Asia. The majority of the Mu sequences (5123) have been detected in North America (55%, n=2841) followed by South America (23%, n=1328), Europe (18%, n=948) and Asia (0.1%, n=6). As of 3 September 2021, Mu has not been detected in Africa. Thus far, it makes up less than 1% of the globally circulating viruses with Delta accounting for 88%.
NGS-SA, which includes the National Institute for Communicable Diseases (NICD), continuously and rigorously monitors SARS-CoV-2 sequences circulating in South Africa. This work is crucial in the early detection of SARS-CoV-2 variants, including Mu.
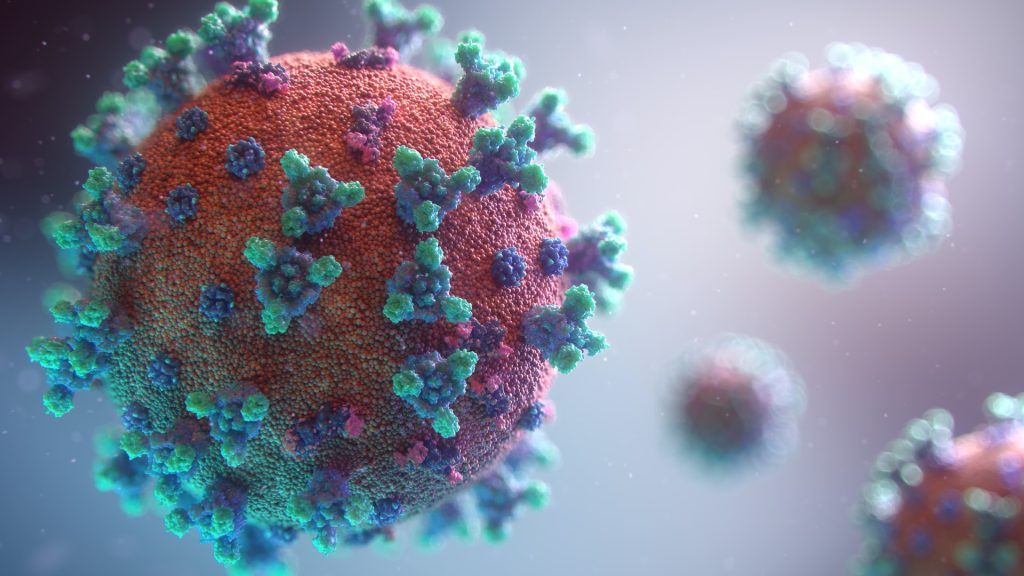
Many of the mutations within the spike protein which define the Mu variant (T95I, E484K, N501Y, D614G, P681H and D950) have been seen before in other VOIs or variants of concern (VOCs) including Beta and Delta. Some of these mutations have previously been associated with decreased antibody responses and increased transmissibility. Therefore it is likely that Mu will have similar properties to other variants with increased transmissibility and reduced sensitivity to antibodies in vaccines and those who have recovered from COVID.
The NICD advises that both COVID vaccines being used in South Africa have high levels of protection against severe disease requiring hospitalisation and death even against VOI/VOCs such as Beta and Delta and therefore will likely also protect against Mu.
Source: NICD