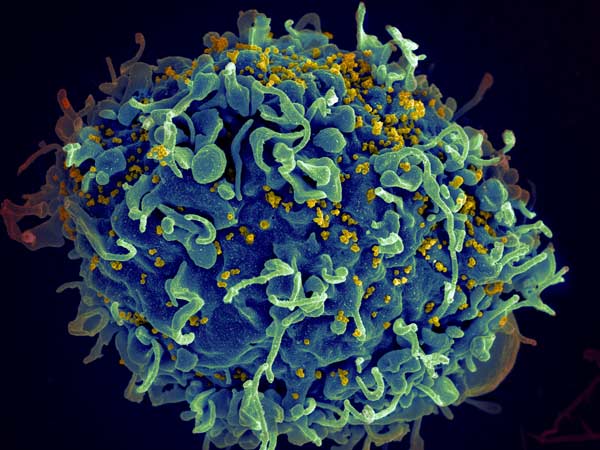
Researchers examining the development of resistance to HIV drugs have uncovered a mechanism of drug resistance development in combination therapy, where ‘windows’ open up for resistance to develop.
In the late 1980s, when HIV treatments were first introduced, patients would often develop resistance to those treatments within six months. The introduction of triple-drug treatment regimens in the 1990s was intended to rectify that. Even if the virus developed resistance to one drug, two others would still knock it out – in theory. Unfortunately, some patients still develop resistance, leaving scientists with a critical question to answer: Why?
“There’s all these things that we still don’t understand, like why do we even get resistance when treating with three drugs,” said San Francisco State University Associate Professor of Biology Pleuni Pennings. “We understand why it is becoming less common, but it should have been zero all along.”
Prof Pennings and her colleagues offer explanations for this phenomenon in a study published in eLife.
Several interesting observations were noted from analysis of HIV patient records. Drug resistance can evolve years after successful therapy, often the result of sequential mutations that occur in a predictable order. Current models could not explain these observations, and while some studies identify mutations that confer drug resistance, they don’t address how and where they arise.
Drawing on two computational models, the researchers suggest that these observations may result from drug heterogeneity over time and throughout the body. While patients receive three HIV therapies simultaneously, drugs have different half-lives and patients do not always adhere to therapy regimens. This could create opportunities for drug resistance evolution, during a window when only one drug is active. Drugs also don’t uniformly penetrate the entire body, meaning that in some locations in a patient’s body, only one of the drugs might be active, creating another evolution and escape opportunity.
“I think one main reason why we should care is actually not because of HIV but because of drug resistance in other situations,” Prof Pennings explained.
Although drug resistance among patients with HIV is fairly low, drug resistance to multidrug therapies is a big problem for diseases such as malaria and tuberculosis. In addition, the COVID pandemic and the rise of variants show how our understanding of evolving pathogens is still lacking.
“In a way, HIV is the poster child of how we solved drug resistance. … [But] if we don’t understand how we did it, then it’s really hard to take these lessons to other situations,” Prof Pennings said.
Source: San Francisco State University

