Investigation of Cannabidiol Oil for Lung Cancer Suggested

In BMJ Case Reports, doctors suggest investigating the use of cannabidiol (‘CBD’) oil as a potential lung cancer treatment, after dealing with a daily user whose lung tumour shrank in the absence of conventional treatment.
The body’s own endocannabinoids are involved in various processes, including nerve function, emotion, energy metabolism, pain and inflammation, sleep and immune function.
Cannabinoids are chemically similar to these, and can interact with signalling pathways in cells, including cancer cells. While they have been studied for use as a primary cancer treatment, there have been inconsistent results.
Despite treatment advances, survival rates for non-small cell lung cancer remain low at around 15% five years after diagnosis, with average survival without treatment is about seven months.
The authors describe the case of a woman in her 80s, a pack-a-week smoker diagnosed with non-small cell lung cancer. The woman also had mild chronic obstructive pulmonary disease (COPD), osteoarthritis, and hypertension, for which she was taking various drugs.
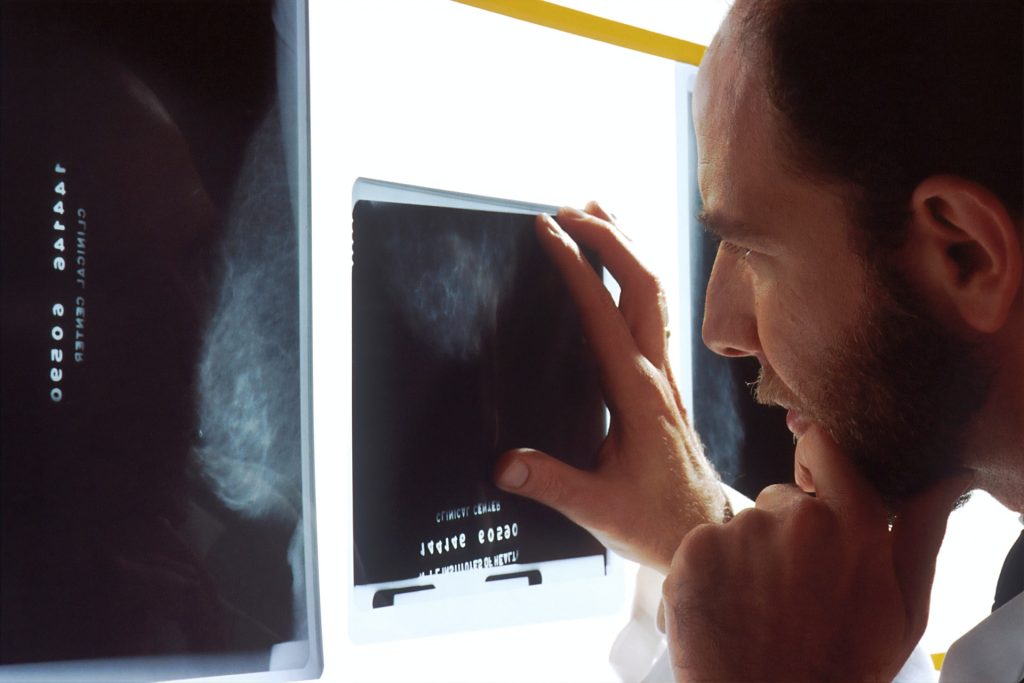
Her tumor was 41 mm in size at diagnosis, with no evidence of local or further spread, so was suitable for conventional treatment of surgery, chemotherapy, and radiotherapy. But the woman refused treatment, so was placed under ‘watch and wait’ monitoring, which included regular CT scans every 3-6 months.
These showed that the tumor was progressively shrinking, reducing in size from 41 mm in June 2018 to 10 mm by February 2021, equal to an overall 76% reduction in maximum diameter, averaging 2.4% a month, say the report authors.
When contacted in 2019 to discuss her progress, the woman revealed that she had been taking CBD oil as an alternative self-treatment for her lung cancer since August 2018, shortly after her original diagnosis.
She had done so on the advice of a relative, after witnessing her husband struggle with the side effects of radiotherapy. She reported consistently taking 0.5 ml of the oil, two to three times a day.
According to the supplier, the main active ingredients were Δ9-tetrahydrocannabinol (THC) at 19.5%, cannabidiol at around 20%, and tetrahydrocannabinolic acid (THCA) at around 24%.
The supplier also said that she should avoid hot food or drinks when taking the oil as she might otherwise feel stoned. The woman reported reduced appetite since taking the oil but had no other obvious ‘side effects’. There were no other changes to her prescribed medications, diet, or lifestyle, and she continued smoking throughout.
The authors cautioned that this is just one case report, with only one other similar case reported, and it is unclear which of the CBD oil ingredients might have been helpful.
“We are unable to confirm the full ingredients of the CBD oil that the patient was taking or to provide information on which of the ingredient(s) may be contributing to the observed tumour regression,” they pointed out.
They further emphasised that, “although there appears to be a relationship between the intake of CBD oil and the observed tumuor regression, we are unable to conclusively confirm that the tumor regression is due to the patient taking CBD oil.”
The authors concluded that, “more research is needed to identify the actual mechanism of action, administration pathways, safe dosages, its effects on different types of cancer and any potential adverse side effects when using cannabinoids.”
Source: News-Medical.Net