T Cells Unnecessary for COVID Recovery

New research with monkeys reveals that primates do not need T cells for the recovery of from acute COVID infections.
T cell depletion was also found not to induce severe disease, and T cells do not explain the natural resistance of rhesus macaques to severe COVID. Furthermore, it was found that strongly T cell-depleted macaques still develop potent memory responses to a second infection.
The findings, published in mBio, an open-access journal of the American Society for Microbiology, have implications for the development of second-generation vaccines and therapeutics.
Lead study author Kim Hasenkrug, PhD, senior investigator in the Laboratory of Persistent Viral Diseases, National Institutes of Health, explained: “We started this study early in the pandemic, trying to figure out how to make a good model to study the disease in humans using animals. The monkeys turned out to be more resistant to the disease than we expected, so we wanted to try to figure out why that was and try to gain some insights into the disease in humans as well. We now know that the antibody response is the most critical response for protection by vaccination, not the T cell response.”
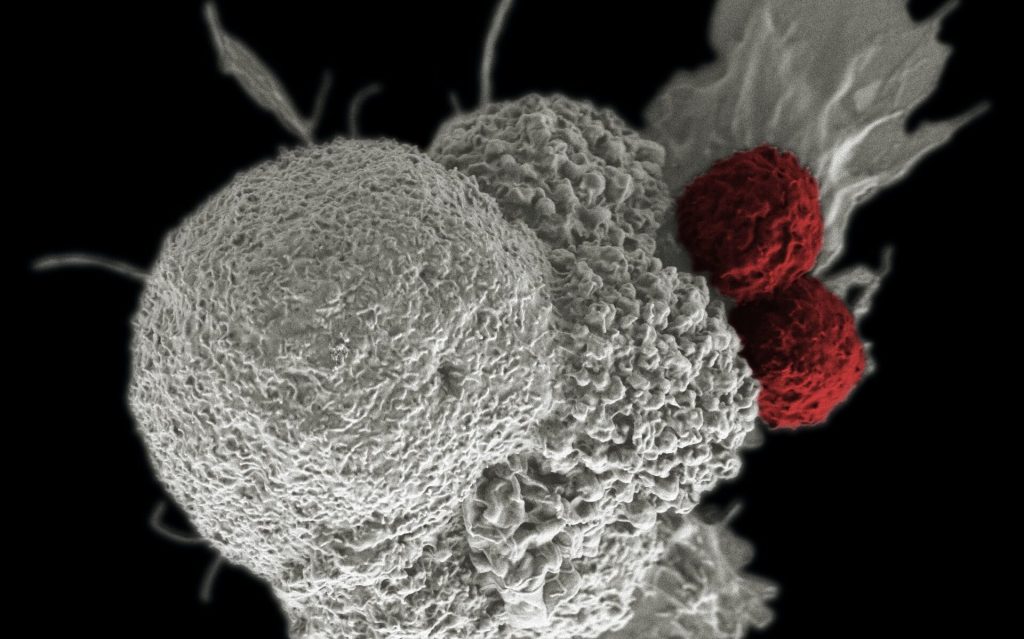
In the new study, the researchers used classic reagents known to deplete CD4+ and CD8+ T cells in rhesus macaques. CD8+ T cells attack infected cells and kill them, and CD4+ T cells are helper T cells that set off the immune response by recognising pathogens and secreting cytokines, which signal other immune cells to act, including CD8+ T cells and antibody-producing B cells.
One week after depleting the macaques of CD4+ T cells, CD8+ T cells, or both at the same time, the researchers infected the animals with SARS-CoV-2. “We depleted, we infected them and then we continued the depletions during the first week of infection to make sure the animals were well depleted. Then we studied their blood to see how they were responding in terms of their T cells and B cells,” said Hasenkrug. Nasal swabs and bronchoalveolar lavages were performed over six weeks to measure virus in the nose, mouth and lungs, along with rectal swabs to check for virus shedding in the gut. After six weeks, the monkeys were re-challenged with SARS-CoV-2 and virus and blood samples collected, which let the researchers evaluate immune memory responses. “If there is a memory response, you get a much quicker immune response and control of the virus. That is how vaccinations work. Once your body has seen a viral pathogen, the next time it sees it, you can get a much faster and stronger immune response,” said Dr Hasenkrug.
Unexpected response
Even with T cell depletion, the monkeys were still able to mount a good memory response against the virus. “We found we got really good memory responses regardless of whether we depleted T cells or not. Basically, we found very strong virus neutralising antibodies, and they are the most important antibodies in controlling the infection. That was unexpected by most immunologists, virologists and vaccinologists,” said Dr Hasenkrug.
“The other thing that happens during a memory response is that antibodies mature, becoming stronger and more potent at binding the viral pathogen. We saw indications of this through what’s called ‘class switching’,” said Dr Hasenkrug.
‘Class switching’ was also not expected in these monkeys with depleted T cells. “We don’t have a firm explanation as to why that happened, but we think it involves some sort of compensatory response, which you can see in our study. For example, when we depleted CD8+ T cells, we saw stronger CD4+ T cell or B cells responses in some animals. When the animals are missing something, they will try to make up for it by making more of something else.”
Dr Hasenkrug doesn’t know why the T cells turned out to be not very important, but this may be a good thing, since people who fail to mount sufficient T cell responses still have opportunities to recover.
“This implies that the innate immune response is critical for initial control of the virus, rather than the adaptive immune responses we studied,” said Hasenkrug.
Source: American Society for Microbiology
Journal information: Hasenkrug, K.J., et al. (2021) Recovery from Acute SARS-CoV-2 Infection and Development of Anamnestic Immune Responses in T Cell-Depleted Rhesus Macaques. mBio. doi.org/10.1128/mBio.01503-21.