A new study published in Nature Communications provides an important new basis for comparing the varying effectiveness of tuberculosis treatments.
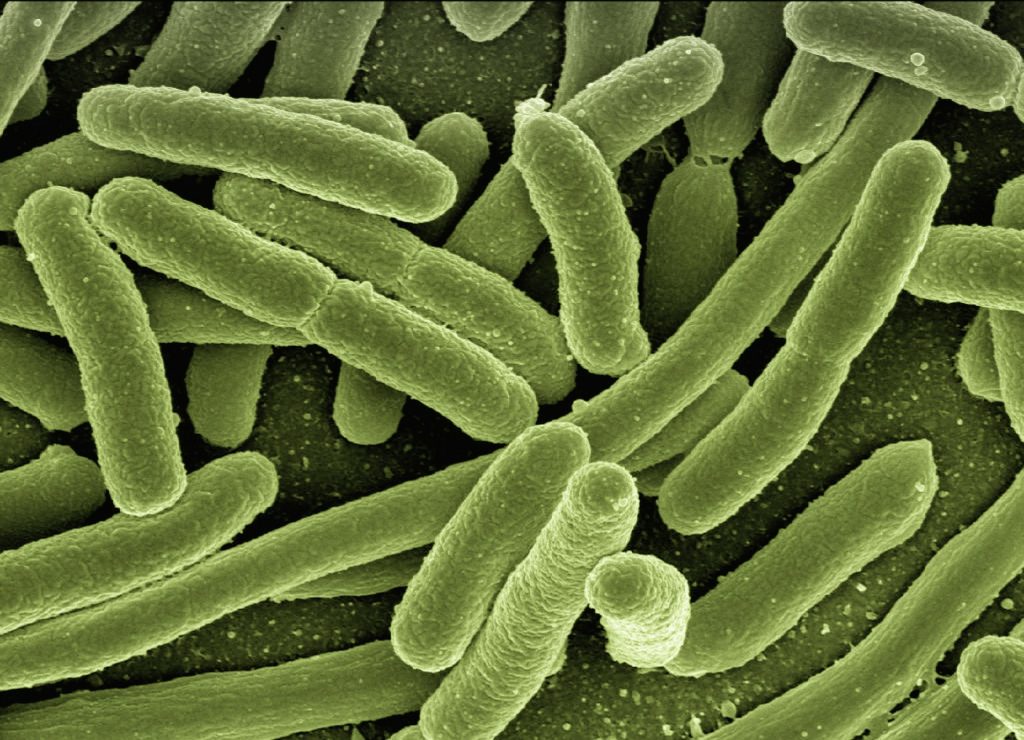
Tuberculosis is a ancient disease caused by the bacterium Mycobacterium tuberculosis (Mtb) and aside from the COVID pandemic, is still the leading infectious cause of death globally, killing 1.2 million people each year. The availability of a new way to evaluate treatments can save lives.
In the study, the researchers aimed to provide a new perspective on assessing the effectiveness of tuberculosis drugs.
“A key roadblock that holds back new tuberculosis treatments is our current inability to accurately measure how effectively different treatments shorten the time needed to cure tuberculosis,” said lead author Nicholas Walter, MD, Ph.D., associate professor at the University of Colorado Anschutz Medical Campus. “Without improved tools to measure and compare the effectiveness of drug treatments, the evaluation and roll-out of new combination drug treatments will continue to proceed slowly.”
“In the past, the effectiveness of tuberculosis treatment has been judged by estimating the burden of the pathogen M. tuberculosis as enumerated via culture based approaches. This historical method correlates poorly with what we care about most, which is whether tuberculosis patients are durably cured,” added co-first author Gregory Robertson, PhD, assistant professor at Colorado State University.

The researchers measured the extent to which drugs interrupt the synthesis of ribosomal RNA, which is needed for the protein-making machinery of the bacterium. They found that drugs and drug regimens that treat tuberculosis faster inhibit Mtb rRNA synthesis more than less potent drugs and regimens. Their resulting new measure, called the rRNA synthesis (RS) Ratio is a useful molecular metric of drug activity based on a key microbial physiologic property rather than a simple measure of reducing bacterial burden.
“The RS Ratio gives us a readout of drug effect that opens a new era in understanding antibiotics. Measuring a key physiologic property of pathogens provides an innovative way of thinking beyond conventional measures of bacterial burden,” said senior author Martin Voskuil, PhD, associate professor at the University of Colorado Anschutz Medical Campus.
“The RS Ratio can enable more intelligent design and evaluation of candidate drug combination regimens, accelerating the development of treatments that can cure tuberculosis faster. This has crucial implications for combatting the global tuberculosis epidemic,” addrf co-author Payam Nahid, MD, MPH, professor and director of the University of California San Francisco Center for Tuberculosis.
Source: Medical Xpress

