A Mediterranean Diet Keeps Dementia at Bay

Researchers have reported that a Mediterranean diet may reduce the risk of developing dementia and cognitive loss, helping preserve memory functions as people age.
Specifically, the diet appears to lower the level of amyloid and tau proteins that are linked with dementia. People following the Mediterranean diet, already noted for its numerous health benefits, scored better on memory tests than those who were not following the diet.
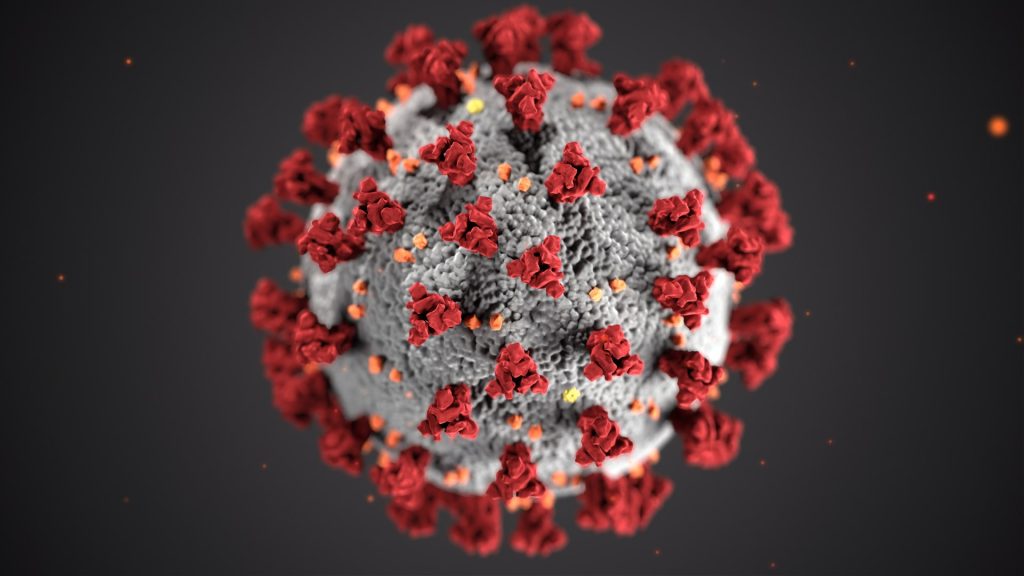
The first of these proteins, amyloid protein, forms plaques in the brain, whereas the second, tau protein, forms tangles. Both are present in the brains of people with Alzheimer’s, though they are not uncommon in the brains of healthy older people, too.
“These results add to the body of evidence that shows what you eat may influence your memory skills later on,” said study author Tommaso Ballarini, PhD, of the German Center for Neurodegenerative Diseases in Bonn, Germany. He adds:
Studies have linked good health with the foods that people living in Greece, Spain, and Italy ate before the 1960s. This diet consists primarily of vegetables and fruits, nuts and seeds, legumes, potatoes, whole grain foods, seafood, extra virgin olive oil, and wine in moderation. Poultry, eggs and dairy products are present to a limited extent, while red meat, added sugar, refined grains and oils, and processed foods are typically lacking in a Mediterranean diet.
Kristin Kirkpatrick, a dietitian at Cleveland Clinic told Medical News Today that the contents of a Mediterranean diet offers beneficial “omega-3 fatty acids, polyphenols, specific minerals, fiber, and protein” that “may support the brain’s health and protection throughout the years.”
However, Kirkpatrick cautioned that, “A diet, even one with strong clinical data on its benefit, is only as healthy as the individuals who choose its structure.”
Sensible portion sizes are important, she noted and warned against the “consumption of processed foods that are marketed as heart-healthy or contain the components seen in a traditional Mediterranean approach.”
The investigators recruited 512 individuals from the German Centre for Neurodegenerative Diseases’ Longitudinal Cognitive Impairment and Dementia StudyTrusted Source. Participant assessments showed that 343 were at a higher risk of developing Alzheimer’s disease while the other 169 people were “cognitively normal.”
Participants filled in questionnaires regarding the food they ate the previous month and the investigators asked them to record their intake of 148 specific food items. Participants were scored on their diet’s similarity to a Mediterranean diet, the most similar receiving a 9 and the least similar a 1. Since this was a self-reported study on eating habits, errors or misrepresentations are possible.
Individuals also took cognitive tests designed to detect the progression of Alzheimer’s disease. The tests assessed five areas: memory, working memory, language, executive functions, and visuospatial abilities. MRI brain scans determined each individual’s brain volume.
Finally, the researchers analyzed spinal fluid from a subsample of 226 participants who gave their consent, assessing the presence and amounts of the two biomarker proteins: amyloid and tau.
After adjusting for sex, age, and education, the scientists identified several clear links between better cognitive health and a Mediterranean diet.
The investigators reported that:
- Every dietary score point lower than 9 was linked to almost 1 year of the brain ageing that occurs in Alzheimer’s disease progression.
- Participants who most closely followed the Mediterranean diet had fewer amyloid and tau protein biomarkers in their spinal fluid than those who had lower dietary scores.
- People on the Mediterranean diet scored better on memory tests than people who were not.
Dr Ballarani concluded that, “More research is needed to show the mechanism by which a Mediterranean diet protects the brain from protein buildup and loss of brain function, but findings suggest that people may reduce their risk for developing Alzheimer’s by incorporating more elements of the Mediterranean diet into their daily diets.”
Source: Medical News Today